When your liver enzymes are high but you don’t drink, don’t smoke, and aren’t overweight, it’s easy to panic. For people with celiac disease, this isn’t rare-it’s common. About 1 in 3 untreated celiac patients show abnormal liver tests, often before they even have digestive symptoms. Many doctors miss the connection, assuming it’s fatty liver or hepatitis. But the real culprit might be gluten-and fixing it doesn’t require pills, just one life-changing change: going completely gluten-free.
Why Your Liver Gets Affected by Gluten
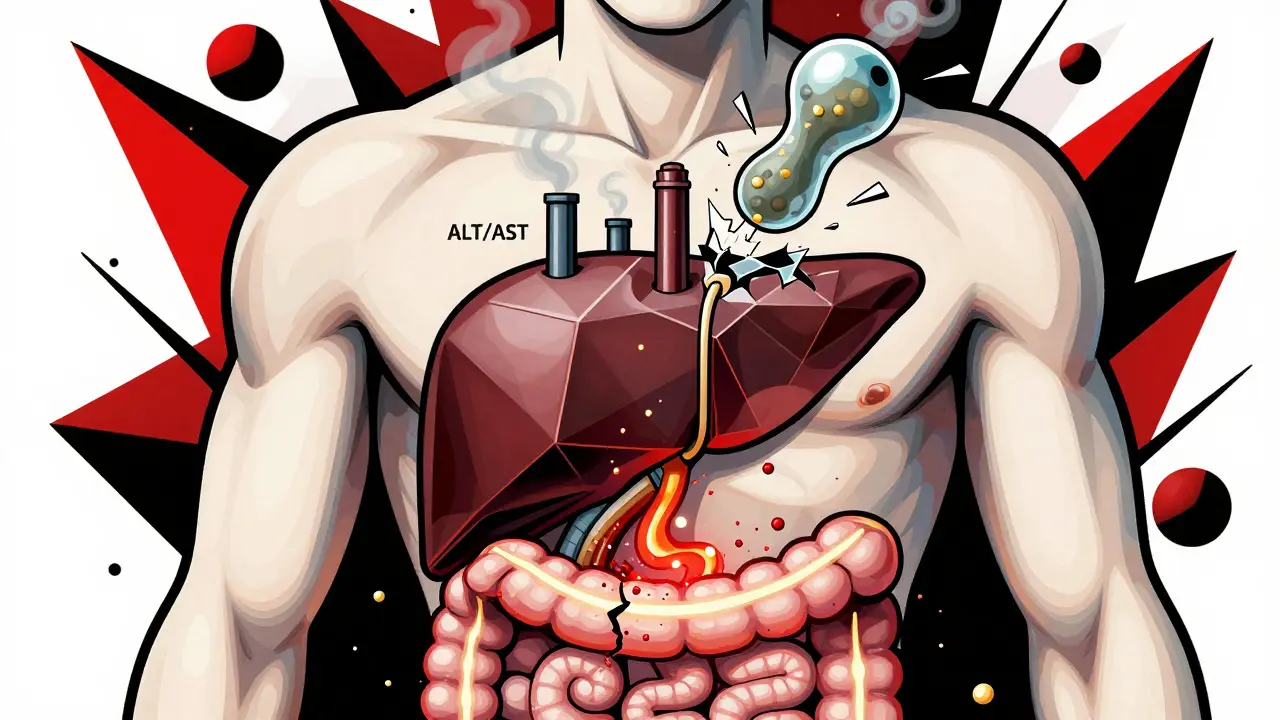
Celiac disease isn’t just a gut problem. It’s an autoimmune disorder where your body attacks its own tissues after eating gluten. That attack usually targets the small intestine, destroying the tiny finger-like projections (villi) that absorb nutrients. But it doesn’t stop there. The same immune chaos can spill over into the liver. Studies show that between 15% and 40% of people newly diagnosed with celiac disease have elevated liver enzymes-mostly ALT and AST. These aren’t random spikes. In 70% of cases, both enzymes rise together, which is a classic sign of liver stress. The liver doesn’t get inflamed because of alcohol or viruses. It gets hit because the gut is leaking. When the intestinal lining is damaged by gluten, it becomes more permeable. Think of it like a sieve with big holes. Toxins, bacteria, and undigested food particles slip through into the bloodstream and head straight to the liver. The liver, your body’s main detox center, tries to clean up the mess. Over time, this constant strain causes inflammation and fat buildup. There’s also an autoimmune link. People with celiac disease are more likely to develop other autoimmune conditions-including autoimmune hepatitis. About 4 to 6 out of every 100 people with autoimmune hepatitis also have undiagnosed celiac disease. The immune system gets confused. It starts attacking liver cells, mistaking them for gluten-triggered invaders.What Liver Problems Are Common With Celiac Disease?
The most frequent issue is elevated liver enzymes. But that’s just the tip of the iceberg. Deeper problems include:- Steatosis (fatty liver): Seen in 25-50% of celiac patients. Fat builds up in liver cells because of poor fat absorption and poor vitamin E and D levels-both needed to protect the liver.
- Autoimmune hepatitis: The immune system attacks liver cells directly. Often misdiagnosed as viral hepatitis.
- Primary biliary cholangitis and primary sclerosing cholangitis: Rarer, but more serious. These affect the bile ducts and can lead to scarring.
- MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease): Formerly called NAFLD. Now, this is a growing concern. Why? Because many gluten-free products are loaded with sugar and refined carbs. People think they’re eating healthy, but they’re gaining weight-and their liver is paying the price.
How High Are the Liver Enzymes? What’s Normal?
Normal ALT levels are usually under 40 U/L. In celiac patients, levels often hit 100-200 U/L-sometimes even higher. That sounds scary, but it’s not like acute hepatitis where enzymes shoot past 1,000. These are mild to moderate elevations, which is why they’re often ignored. The pattern matters:- Both ALT and AST elevated? Likely celiac-related.
- ALT alone elevated? Still possible, especially if you’re not drinking.
- AST higher than ALT? Could point to alcohol or advanced liver damage.
The Gluten-Free Diet: The Only Treatment You Need
This is the most important part: for most people, the liver fixes itself-no medication, no surgery, just cutting out gluten. A 2015 study by Dr. Daniel Leffler tracked 100 celiac patients with elevated liver enzymes. After 18 months on a strict gluten-free diet, 79% saw their enzymes return to normal. Another study found that 85% normalized within 12 months. That’s not a coincidence. It’s proof that the liver damage was caused by gluten, not something permanent. But here’s the trap: not all gluten-free diets are equal. Many packaged gluten-free foods are full of refined rice flour, potato starch, sugar, and unhealthy fats. People lose weight on gluten-free diets? Sometimes. But many gain it-because they’re eating more processed junk. And that’s how MASLD creeps in. A 2023 study from the Celiac Disease Foundation showed that patients who worked with a celiac-specialized dietitian normalized their liver enzymes 30% faster than those who just got generic advice. Why? Because the dietitian taught them to eat whole foods: vegetables, lean meats, eggs, nuts, quinoa, buckwheat, and naturally gluten-free grains like millet and amaranth.
What If Your Liver Enzymes Don’t Improve?
If your enzymes are still high after 12 months of strict gluten avoidance, it’s time to dig deeper. You might have another condition hiding alongside celiac disease.- Check for autoimmune hepatitis with an ANA and anti-smooth muscle antibody test.
- Rule out primary biliary cholangitis with an AMA test.
- Get a liver ultrasound or FibroScan to check for fat or scarring.
- Test for vitamin D, E, and zinc levels-low levels worsen liver damage.
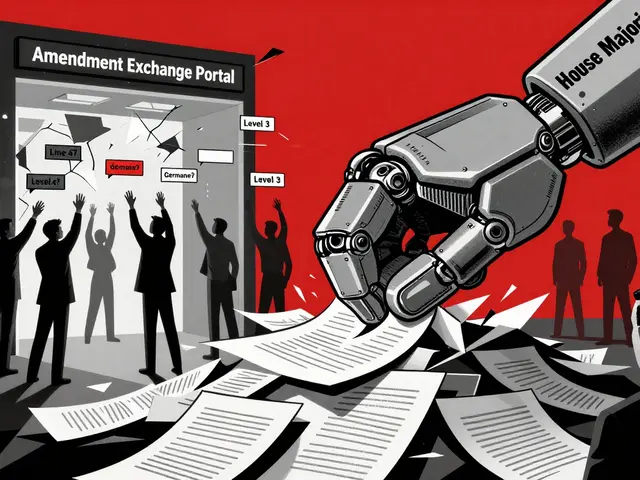
How Doctors Are Changing Their Approach
Ten years ago, most doctors didn’t check liver enzymes when diagnosing celiac disease. Now, 92% do. That’s because research made it impossible to ignore. In June 2024, the European Association for the Study of the Liver updated its guidelines: all patients with unexplained cirrhosis should be screened for celiac disease. Why? Because 1 in 20 of those patients had it-and their liver improved after going gluten-free. Pharmaceutical companies are also paying attention. Takeda Pharmaceutical completed a Phase II trial in late 2023 testing an enzyme that breaks down gluten in the stomach. If it works, it could reduce liver inflammation in people who accidentally ingest gluten. And researchers at the University of Helsinki are tracking 500 celiac patients over 10 years to see if longer gluten exposure before diagnosis leads to worse liver damage. Early data suggests it does.What You Should Do Right Now
If you have celiac disease and your liver enzymes are high:- Get a full liver panel: ALT, AST, ALP, GGT, bilirubin, albumin.
- Start a whole-food, unprocessed gluten-free diet immediately. Avoid gluten-free cookies, crackers, and pastas for now.
- See a dietitian who specializes in celiac disease-don’t guess.
- Get tested for autoimmune liver diseases if enzymes don’t drop in 6 months.
- Check your vitamin D and E levels. Supplement if needed.
- Repeat liver tests every 3-6 months until normal.
Real Stories, Real Results
One Reddit user, diagnosed with celiac in 2023, wrote: “My ALT was 142. My doctor said I had fatty liver. I was scared. Then I found out I had celiac. I went gluten-free. Six months later, my ALT was 38. I felt better than I had in years.” Another woman, 54, had unexplained fatigue and elevated enzymes for two years. No one linked it to her gluten sensitivity. After her diagnosis, she dropped 18 pounds-not because she was dieting, but because her body stopped absorbing toxins. Her liver healed. Her energy came back. These aren’t outliers. They’re the norm.What’s Next for Research?
Scientists are now looking for genetic markers that predict who’s most at risk. Early findings suggest people with two copies of the HLA-DQ2 gene (homozygous) are 2.3 times more likely to develop liver problems than those with just one copy. That could lead to early screening for high-risk kids before symptoms even start. The goal? Stop liver damage before it begins. Not just treat it after it’s there.Final Thought: Your Liver Can Heal
You don’t need a miracle drug. You don’t need surgery. You don’t need to spend thousands on supplements. Just stop eating gluten-completely, consistently, and wisely. The liver is one of the few organs that can regenerate. If you give it a chance, it will. But you have to remove the poison. And for people with celiac disease, that poison is gluten. Don’t wait for symptoms to get worse. Don’t assume your liver issue is just “fatty liver.” Ask the question: Could this be celiac?Can celiac disease cause elevated liver enzymes even without digestive symptoms?
Yes. Many people with celiac disease have no stomach pain, bloating, or diarrhea when first diagnosed. Instead, their only sign is abnormal liver enzymes-sometimes discovered during a routine blood test. This is why liver function tests are now part of standard celiac screening.
Will my liver enzymes return to normal on a gluten-free diet?
In most cases, yes. About 79% of people with celiac disease and elevated liver enzymes see normal levels within 12 to 18 months of strictly avoiding gluten. The liver has a strong ability to repair itself once the trigger is removed.
Can a gluten-free diet cause fatty liver?
Yes, if you rely on processed gluten-free foods. Many of these products are high in sugar, refined starches, and unhealthy fats. Eating too many of them can lead to weight gain and MASLD (fatty liver), even if you’re avoiding gluten. The key is to focus on whole, unprocessed foods like vegetables, lean meats, nuts, and naturally gluten-free grains.
Should I be tested for celiac disease if I have unexplained fatty liver?
Yes, especially if you’re not overweight, don’t drink alcohol, and have no clear cause for your fatty liver. Studies show that 4.7% of people with unexplained cirrhosis have undiagnosed celiac disease. A simple blood test for tTG-IgA antibodies can rule it in or out.
How long does it take for liver enzymes to improve after going gluten-free?
Most people see improvement within 3 to 6 months. Normalization typically happens between 12 and 18 months. If enzymes haven’t dropped after a year, your doctor should check for other liver conditions like autoimmune hepatitis or primary biliary cholangitis.
Do I need a liver biopsy if I have celiac disease and high enzymes?
Usually not. Most liver changes in celiac disease are reversible with diet alone. A biopsy is only recommended if enzymes stay high after 12 months of strict gluten-free eating, or if other signs suggest advanced liver disease like scarring or bile duct damage.



The liver-celiac link is so under-discussed. I had ALT at 189 and was told I had NAFLD. Turned out I had silent celiac. Went gluten-free. 14 months later, normal. No meds. No miracle. Just stop eating the poison. This isn't alternative medicine-it's basic physiology.
January 12Doctors still treat symptoms, not causes. That's why people stay sick.
Lauren Warner