Rheumatoid arthritis isn't just stiff joints or achy hands. It’s your own immune system turning against you-attacking the lining of your joints, triggering inflammation that can destroy cartilage, erode bone, and leave you struggling to button a shirt or open a jar. Unlike osteoarthritis, which comes from wear and tear, RA is an autoimmune disease. That means something in your body’s defense system has gone rogue, and it’s not just hurting your joints-it can hit your lungs, heart, eyes, and even your blood vessels.
How Rheumatoid Arthritis Actually Works
Inside your joints, there’s a thin layer of tissue called the synovium. It’s supposed to make fluid that keeps your joints moving smoothly. In RA, your immune system mistakes this tissue for a threat. It sends immune cells and inflammatory chemicals straight to your joints. The result? Swelling, heat, pain, and over time, permanent damage.
This doesn’t happen overnight. Most people notice symptoms slowly-maybe a few stiff fingers in the morning, or aching knuckles that won’t go away after a week. But if it lasts more than six weeks, especially with swelling in the same joints on both sides (like both wrists or both knees), it’s a red flag. Morning stiffness lasting 45 minutes or longer is a classic sign. By the time you see your doctor, the damage may already be underway.
Doctors use blood tests to help confirm it. Two key markers are rheumatoid factor (RF) and anti-CCP antibodies. If you test positive for anti-CCP, there’s a high chance you have RA-even before joint damage shows up on an X-ray. Imaging like ultrasound or MRI can catch early inflammation before bones start to erode.
Women are two to three times more likely to get RA than men. It usually starts between ages 30 and 60, but it can hit younger people too. Genetics play a role-certain versions of HLA genes increase risk-but environment matters just as much. Smoking, exposure to silica dust, and even certain infections may trigger the disease in people who are genetically vulnerable.
Why Early Treatment Changes Everything
There’s a narrow window-roughly the first three to six months after symptoms start-where you can stop RA from causing irreversible damage. After that, joint destruction becomes harder to reverse. That’s why experts call it the "window of opportunity."
Early, aggressive treatment isn’t optional. It’s the difference between being able to keep working, playing with your kids, or holding a cup of coffee, and ending up with deformed hands or needing joint replacements before you’re 50.
The goal isn’t just to feel better-it’s to reach remission. That means no signs of active disease. Even low disease activity is a win. Studies show that people who reach remission within a year have far less long-term disability.
Doctors use a "treat-to-target" approach: check your disease activity every few months, adjust meds if needed, and keep pushing until you hit the target. It’s not a set-it-and-forget-it plan. It’s active management.
First-Line Treatment: Methotrexate
Before you even think about biologics, most patients start with methotrexate. It’s been the backbone of RA treatment for decades. It’s cheap, effective, and well-studied. About 68% of new RA patients get it as their first drug.
Methotrexate works by calming down the whole immune system. It doesn’t target one specific molecule-it slows the overall inflammatory response. Side effects include nausea, fatigue, and liver stress, so you’ll need regular blood tests. But for many, it’s enough to control symptoms and slow damage.
Still, about 40% of people don’t respond well enough. That’s when doctors turn to biologics.
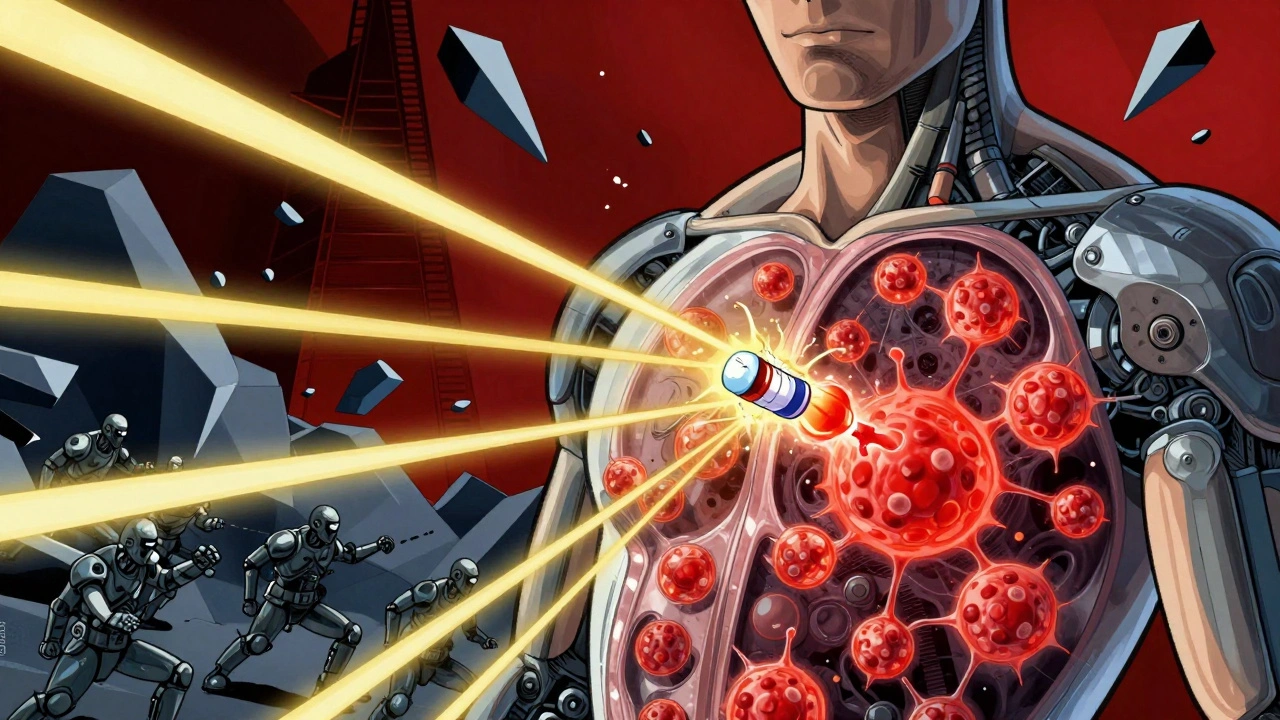
What Are Biologic Therapies?
Biologics are a class of drugs made from living cells-usually proteins-that target very specific parts of the immune system. Unlike methotrexate, which is broad-acting, biologics are like precision missiles. They block just the molecules driving inflammation in RA.
The first one, etanercept, got FDA approval in 1998. Since then, we’ve seen a revolution. Today, biologics are used in about one-third of RA patients.
There are four main types:
- TNF inhibitors (like adalimumab, etanercept, infliximab): Block tumor necrosis factor, a major inflammatory protein. These are the most commonly prescribed biologics, making up 55% of all biologic use.
- IL-6 inhibitors (like tocilizumab): Stop interleukin-6, another key player in joint damage. Used when TNF blockers don’t work.
- B-cell inhibitors (like rituximab): Deplete B-cells, the immune cells that produce harmful antibodies in RA.
- T-cell costimulation blockers (like abatacept): Prevent T-cells from activating other immune cells.
Studies show that when you combine a biologic with methotrexate, about 60% of patients see a 50% or greater drop in disease activity. That’s compared to 40% with methotrexate alone.

Real People, Real Results
Sarah K., 42, stopped playing piano five years ago because her fingers were too swollen and bent. She tried multiple drugs, but nothing helped. After starting tocilizumab in 2022, she noticed her hands felt lighter. Within six months, she could hold a pen again. A year later, she played a full song for her family for the first time in years.
But not everyone has that story. On patient forums like Reddit’s r/rheumatoidarthritis, many share frustration. One user said, "I’ve been on Humira for two years. It helps, but I’m tired of getting sick every winter." Another wrote, "I had to quit my job because I couldn’t afford the copay."
Drugs.com data shows Humira gets a 6.5 out of 10 average rating. About 48% of users say it significantly improved their life. But 32% report injection site reactions-redness, itching, or pain where the shot goes in. And 37% of biologic users say they’ve had serious infections-pneumonia, skin abscesses, even tuberculosis reactivation.
The Hidden Costs: Money, Access, and Mental Health
Biologics aren’t just expensive-they’re financially crushing. Annual costs range from $15,000 to $60,000. Even with insurance, out-of-pocket costs can hit $5,000 a year. A 2023 Arthritis Foundation survey found 41% of patients skipped doses or delayed refills because of cost. Over half said the financial burden affected their mental health.
And access isn’t equal. Rural patients are 30% less likely to get biologics than those in cities. Why? Fewer rheumatologists, longer travel times, and insurance hurdles.
There’s some hope. The first biosimilar to adalimumab (adalimumab-adaz) was approved in September 2023. Biosimilars are nearly identical to the original drug but cost 15-20% less. More are coming. That could make treatment more accessible.
Side Effects and Risks
Biologics weaken parts of your immune system. That’s how they help RA-but it also means you’re more vulnerable to infections.
You need a TB test before starting. If you’ve had hepatitis B, it can flare up. You should avoid live vaccines (like the shingles vaccine) while on biologics. If you develop a fever, cough, or unusual fatigue, call your doctor right away.
There’s also a small increased risk of lymphoma-about 1 in 1,000 patients over 10 years. That sounds scary, but it’s still rarer than the risk from uncontrolled RA itself. The bigger risk? Letting RA run wild.
Every biologic comes with a FDA-mandated Risk Evaluation and Mitigation Strategy (REMS). That means your doctor has to educate you on infection signs, and you have to sign off on understanding the risks.

What’s Next? New Drugs and Better Predictions
Science is moving fast. In January 2024, the FDA approved upadacitinib (Rinvoq) for early RA. It’s a JAK inhibitor-a newer type of targeted drug that works inside cells, not just on their surface. It’s taken 15% of the biologic market in just two years.
Researchers are also working on ways to predict who will respond to which drug. The Accelerating Medicines Partnership found they could predict methotrexate response with 85% accuracy using genetic markers. Imagine knowing upfront whether a drug will work for you-no trial and error.
Next up: TYK2 inhibitors like deucravacitinib. These are oral pills that target a different pathway than JAK inhibitors. They’re in phase 3 trials and could be available by 2026.
Living With RA: Beyond Medication
Medication is critical-but it’s not the whole story. Exercise matters. The CDC recommends 150 minutes of moderate activity per week-walking, swimming, cycling. Studies show it reduces pain and stiffness without worsening damage.
Weight loss helps too. Losing just 5-10% of your body weight can cut disease activity by 20-30%. For someone who’s overweight, that’s a game-changer.
Support groups make a difference. The Arthritis Foundation’s Live Yes! Network has 100,000 members. Their self-management workshops reduce pain by 20% in six months. Apps like MyRA help track symptoms, meds, and flare triggers.
And sleep? Crucial. Poor sleep worsens inflammation. Stress management-through yoga, mindfulness, or therapy-can lower flare frequency.
Final Thoughts: You’re Not Alone
Rheumatoid arthritis is lifelong. It’s unpredictable. Some days you’ll feel fine. Others, you won’t be able to get out of bed. But it’s not a death sentence. With early diagnosis, the right treatment, and smart self-care, you can live well.
The tools are here. Biologics, biosimilars, JAK inhibitors, and better diagnostics are giving people back their lives. The challenge now is making them accessible-not just to those who can afford it, but to everyone who needs them.
If you’re dealing with joint pain that won’t go away, don’t wait. See a rheumatologist. Ask about testing. Push for early treatment. Your future self will thank you.
Is rheumatoid arthritis the same as osteoarthritis?
No. Osteoarthritis is caused by wear and tear on joints over time-like cartilage breaking down from age or injury. Rheumatoid arthritis is an autoimmune disease where your immune system attacks your joints. RA causes inflammation, swelling, and systemic symptoms, while osteoarthritis is localized and doesn’t involve the immune system.
Can biologics cure rheumatoid arthritis?
No, biologics can’t cure RA. But they can put the disease into remission-meaning no signs of active inflammation. Many people stay in remission for years and live without joint damage. Stopping treatment often leads to a flare, so most people need to stay on medication long-term.
How long does it take for biologics to work?
It varies. Some people feel better in 2-4 weeks. For others, it takes 3-6 months to see full effects. TNF inhibitors often work faster than B-cell or T-cell blockers. Your doctor will monitor your progress with blood tests and symptom tracking to see if it’s working.
Are biologics safe if I want to get pregnant?
Some biologics are considered safe during pregnancy. Etanercept and adalimumab have the most data supporting their use. Others, like rituximab, are avoided. Always talk to your rheumatologist before trying to conceive. You may need to switch medications or adjust timing to protect both you and your baby.
What happens if a biologic stops working?
It’s common for biologics to lose effectiveness over time. This is called secondary failure. If that happens, your doctor may switch you to another biologic-often from a different class-or add a JAK inhibitor. Some people respond better to IL-6 inhibitors after failing TNF blockers. There’s no one-size-fits-all, but there are multiple options.
Can I take biologics with other medications?
Yes, most people take biologics with methotrexate for better results. But you should avoid combining them with other strong immune suppressants like corticosteroids long-term, unless absolutely necessary. Always tell your doctor about every medication, supplement, or herb you’re taking-some can interact or increase infection risk.
Do biologics cause weight gain?
Biologics themselves don’t directly cause weight gain. But if they reduce your pain and inflammation, you might become more active, which could help with weight loss. On the flip side, if you’re taking high-dose steroids along with a biologic, that can lead to weight gain. Weight changes are usually tied to other meds or lifestyle, not the biologic itself.
What’s the difference between a biologic and a biosimilar?
A biologic is the original drug made by the company that developed it-like Humira (adalimumab). A biosimilar is a highly similar version made after the original patent expires. It’s not a generic-it’s more complex to produce-but it works the same way and is FDA-approved as safe and effective. Biosimilars cost less, making treatment more affordable.





RA is brutal but treatable. I started on methotrexate and it barely touched my symptoms. Switched to adalimumab and within three months my hands stopped locking up. Still get morning stiffness but now I can hold a coffee cup without crying. Don’t give up if the first drug fails. It’s a marathon not a sprint.
December 2Also please get a biosimilar if you can. Same drug half the price. No reason to pay full retail when the science says it’s identical.
Wendy Chiridza