It starts with a rash. Maybe it’s itchy, red, and flaky where you applied your cream or ointment. You think, “This is just irritation,” so you keep using it-maybe even double down because you were told it would help. But the rash spreads. It burns. It won’t go away. And then you realize: the medicine you’re using to treat your skin might be the thing making it worse.
This isn’t rare. About 1 in 6 people who get patch-tested for stubborn skin rashes turn out to be allergic to something in their topical medication. That’s not a fluke. It’s a pattern. And it’s often missed-because doctors, and patients, assume the treatment can’t be the problem. But it can be. And when it is, the wrong treatment makes everything worse.
What’s Really Going On? Irritation vs. Allergy
Not every rash from a cream is an allergy. There are two kinds of reactions you need to tell apart.
Irritant contact dermatitis is the most common. It happens when something physically damages your skin-like soap, alcohol, or even too much scrubbing. It doesn’t need your immune system to get involved. It just burns or chafes the surface. This kind usually shows up fast, right after you apply the product, and it’s often limited to the area you touched.
Allergic contact dermatitis is different. It’s a delayed immune reaction. Your body has seen the substance before-maybe you used it last year, or your aunt used it on her eczema-and now your immune system remembers it like a threat. The next time you apply it, your skin doesn’t react right away. It takes 24 to 72 hours. That’s why people think, “It’s not the cream, I used it yesterday and nothing happened.” But by day three, the red, blistering, itchy rash shows up. And it can spread beyond where you applied it.
Here’s the kicker: 15% to 20% of people who think they’re allergic to a topical medication are actually just dealing with irritation. The rest? They’ve got a true allergy. And if you don’t know which one it is, you’re treating the wrong problem.
What Medications Cause Allergies? The Top Suspects
There are over 360 drugs that can trigger allergic contact dermatitis. But a handful show up again and again in patch tests.
- Antibiotics-especially neomycin. Found in over-the-counter first-aid creams, wound ointments, and even some prescription dressings. It’s the #1 offender, showing up in nearly 1 in 10 positive patch tests.
- Corticosteroids-yes, the very drugs doctors prescribe to calm rashes. Hydrocortisone, triamcinolone, betamethasone. About 1 in 50 people using these develop an allergy to them. That’s a cruel twist: you’re using a steroid to treat eczema, and it ends up making your eczema worse.
- Local anesthetics-like benzocaine, often in numbing sprays, teething gels, and hemorrhoid creams. Easy to miss because it’s not labeled as a “medication” on the bottle.
- NSAIDs-topical pain relievers like ketoprofen (used in gels for muscle pain) are sneaky allergens. People think they’re safe because they’re “natural” or “non-steroidal.” They’re not.
And here’s the hidden danger: cross-reactivity. If you’re allergic to one steroid, you might react to others-even if they’re different brands. Steroids are grouped into categories (A through F). If you’re allergic to Group A (like hydrocortisone), you can usually use Group B (triamcinolone) or Group D (methylprednisolone aceponate) safely. But without knowing your group, you’re just guessing.
How Do You Know for Sure? Patch Testing Explained
There’s no blood test for topical medication allergies. The only reliable way to find out what’s causing your rash is patch testing.
Here’s how it works: Small amounts of common allergens-including a panel of 30+ topical medications-are taped to your back in tiny chambers. You leave them on for 48 hours. Then the patches come off. You come back at 72 hours and again at 96 hours. That’s when the allergic reaction shows up. It’s slow, because your immune system is slow to react.
When done right, patch testing identifies the culprit in about 70% of cases. But here’s the problem: most GPs don’t do it. You’ll likely need to see a dermatologist or allergist who specializes in contact dermatitis. And if you’ve been using multiple creams, ointments, and lotions over the years, bring them all. Thirty percent of allergens are hiding in things you don’t even think of as medicine-fragranced moisturizers, sunscreen, even baby wipes.
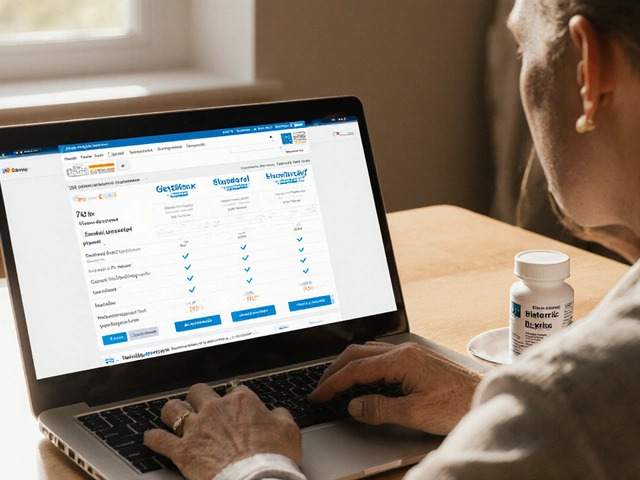
There’s an app now-made by the American Contact Dermatitis Society-that lets you scan product barcodes and see if they contain common allergens. Over 40% of patch-tested patients use it to avoid hidden triggers.
Treatment: Stop the Allergen, Then Soothe the Skin
The most important step? Stop using the allergen. That’s it. No fancy drugs. No magic cure. Just avoidance.
Studies show that 89% of people with contact dermatitis see their rash clear up completely within four weeks-only if they stop using the triggering substance. If they keep using it, even with steroids, the rash lingers for months. Or worse-it gets worse.
Once you’ve stopped the allergen, here’s what works:
- Mild cases: Over-the-counter 1% hydrocortisone cream, twice a day for up to a week. If it doesn’t help in 5 days, see a doctor.
- Moderate to severe: Prescription corticosteroids like triamcinolone 0.1% or clobetasol 0.05%. But here’s the catch-don’t use strong steroids on your face, eyelids, or groin. Those areas are thin. Long-term use can cause skin thinning, stretch marks, or even permanent damage. Use desonide or low-potency options instead.
- Large areas (over 20% of your body): Oral prednisone. Usually 40-60 mg a day for 2-3 weeks, then slowly tapered. Most people feel better within 12-24 hours.
- Sensitive areas or steroid-sparing: Tacrolimus (Protopic) or pimecrolimus (Elidel). These are calcineurin inhibitors. They’re not steroids, so no skin thinning. They work well-60-70% of users see improvement. But they can burn at first. That’s normal. It fades after a few days.
And yes-some people get allergic to calcineurin inhibitors too. It’s rare, but it happens. That’s why patch testing matters. You need to know what’s safe before you try it.
The Hidden Cost of Misdiagnosis
Most people with topical medication allergies see 3 or more doctors before getting the right diagnosis. On average, they suffer for 6 months. One Reddit user described it as “being trapped in a loop: doctor gives me steroid, rash gets worse, I get another steroid, it gets worse again.”
Healthcare workers are especially at risk. About 18% of nurses and aides develop contact dermatitis from gloves, antiseptics, or topical meds they use daily. Many don’t report it because they think it’s just “dry skin.”
And the financial cost? The global market for contact dermatitis treatments hit $2.8 billion in 2022. A lot of that money is spent on treatments that make the problem worse because the root cause isn’t found.
What You Can Do Today
Don’t wait for a rash to turn chronic. Here’s your action plan:
- Stop using any new cream or ointment that started right before the rash appeared-even if your doctor prescribed it.
- Write down everything you’ve applied to the skin in the last 3 months: prescriptions, OTC products, lotions, sunscreens, even makeup.
- Take photos of the rash. Note where it started, how it changed, and what you did each day.
- Ask your dermatologist for patch testing. Don’t accept “it’s just eczema” or “you’re overusing steroids.” Say: “I think I might be allergic to something in my treatment.”
- Download the ACDS app and scan your products. You might be surprised what’s in them.
If you’ve been stuck with a rash for months, and nothing seems to help, the answer might not be stronger medicine. It might be stopping the medicine altogether.
Frequently Asked Questions
Can you become allergic to a topical medication you’ve used for years?
Yes. Allergic contact dermatitis is a delayed immune response that builds up over time. You can use a cream safely for months-or even years-then suddenly react. This is why it’s often mistaken for a flare-up of eczema or psoriasis. Your immune system didn’t recognize the substance as a threat until now.
Is hydrocortisone safe if I’m allergic to steroids?
Not if you’re allergic to Group A corticosteroids, which includes hydrocortisone and hydrocortisone butyrate. Even low-dose OTC hydrocortisone can trigger a reaction in these patients. If you’ve had a rash after using hydrocortisone, avoid all Group A steroids. Talk to your dermatologist about steroid groups to find safe alternatives.
Can patch testing be done on children?
Yes. Patch testing is safe for children over age 6, especially if they have chronic eczema that isn’t improving with standard treatments. Pediatric dermatologists use smaller patches and adjust the allergen panel based on the child’s exposure history. It’s often the missing piece in treatment-resistant cases.
How long does it take for a rash to clear after stopping the allergen?
Itching usually improves within 48 to 72 hours. Redness and swelling take 1-2 weeks to fade. Complete healing can take 2-4 weeks, especially if the skin was broken or infected. Avoid scratching-it delays healing and increases infection risk. Moisturizing with a fragrance-free barrier cream helps speed recovery.
Are natural or herbal topical products safer?
No. Many plant-based ingredients like tea tree oil, lanolin, and fragrances from essential oils are common allergens. In fact, 30% of positive patch tests come from “natural” or “organic” products. Just because something is labeled “natural” doesn’t mean it’s safe for sensitive skin. Always patch test new products, even if they’re marketed as gentle.



Topical medication allergies are a well-documented phenomenon in dermatological literature, with patch testing remaining the gold standard for diagnosis. The prevalence of neomycin and corticosteroid sensitization is consistently reported across multiple peer-reviewed studies. Avoidance remains the most effective intervention, with resolution rates exceeding 85% when triggers are eliminated. The utility of the ACDS app for consumer education is commendable and aligns with evidence-based practice.
November 20Cooper Long