When you have Parkinson’s disease, nausea isn’t just an inconvenience-it’s a common side effect of your life-saving meds. About 40 to 80% of people starting levodopa experience it. But treating that nausea can be dangerous. Many antiemetics block dopamine receptors to stop vomiting. And in Parkinson’s, your brain is already starved of dopamine. Giving a drug that blocks what little dopamine you have left can make your tremors worse, freeze your movements, or send you into a severe ‘off’ episode.
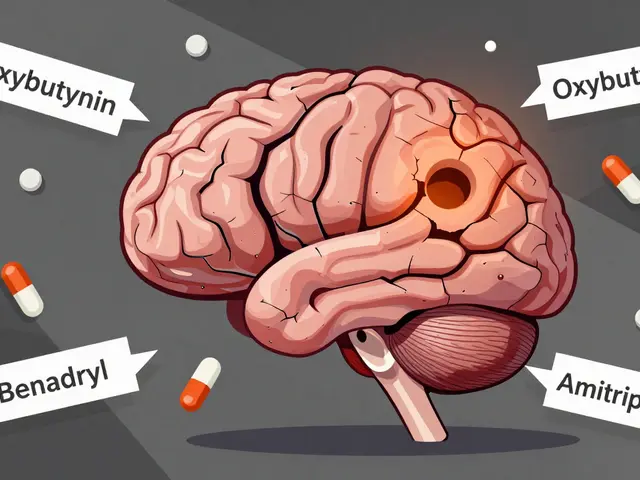
Why Dopamine Antagonists Are a Problem
Parkinson’s isn’t just about shaking hands. It’s about dying nerve cells in the substantia nigra, the part of your brain that makes dopamine. Levodopa replaces that lost dopamine. But antiemetics like metoclopramide, prochlorperazine, and haloperidol work by sticking to dopamine D2 receptors-same receptors levodopa needs to work. When these drugs get into your brain, they compete with levodopa. They don’t just reduce nausea-they reduce your ability to move.It’s not theoretical. A 2022 survey by the Michael J. Fox Foundation found 68% of Parkinson’s patients who got dopamine-blocking antiemetics in the hospital reported a sharp decline in mobility. One patient on Reddit described being given metoclopramide after dental surgery: “My tremors went from mild to uncontrollable. It took three weeks to get back to normal, even after upping my levodopa.”
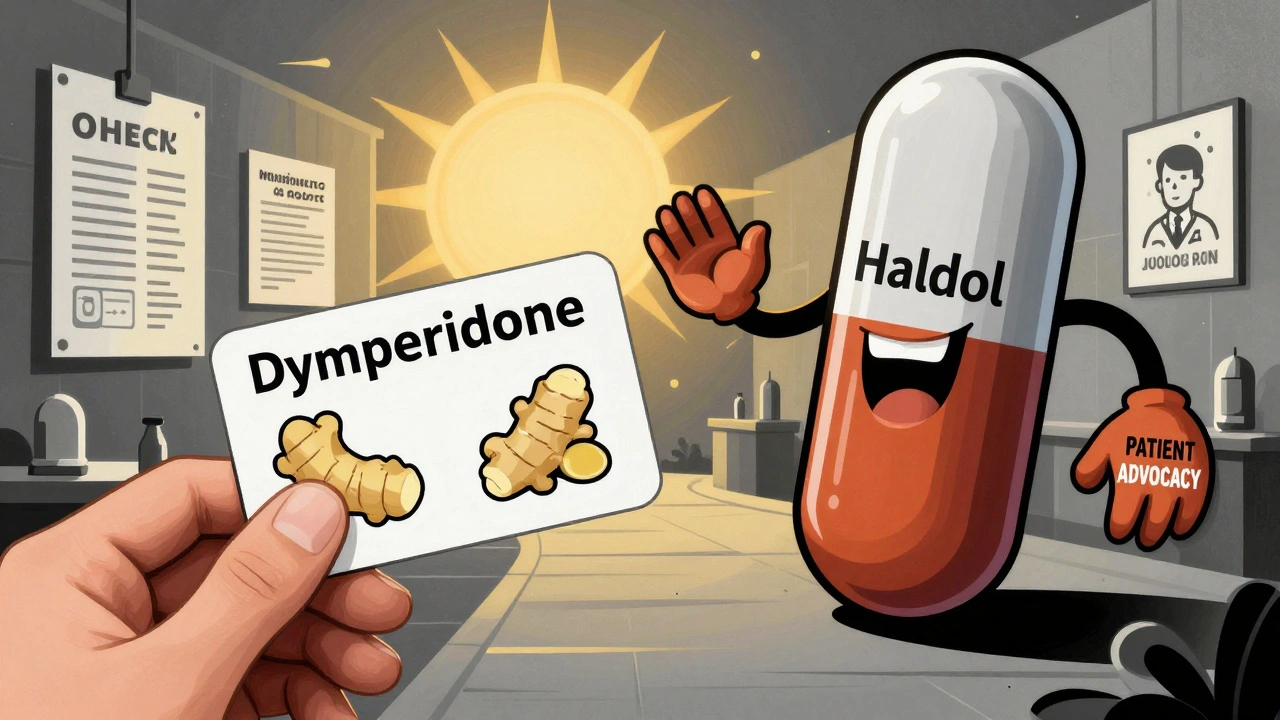
Not All Antiemetics Are Created Equal
The difference between safe and dangerous isn’t always obvious. It comes down to one thing: can the drug cross the blood-brain barrier?High-risk drugs (cross the barrier easily):
- Metoclopramide (Reglan, Maxalon)
- Prochlorperazine (Stemetil)
- Haloperidol (Haldol)
- Chlorpromazine
- Promethazine
These are common in ERs and post-op settings. But for Parkinson’s patients, they’re a ticking time bomb. The American Parkinson Disease Association lists them as medications to avoid. Metoclopramide, despite being widely used for nausea, has a 95% risk of worsening symptoms according to their 2023 guidelines.
Lower-risk alternatives (mostly stay outside the brain):
- Domperidone (Motilium)
- Cyclizine (Vertin)
- Ondansetron (Zofran)
Domperidone is the gold standard for Parkinson’s patients. It blocks dopamine receptors in the gut-where nausea starts-but can’t reach the brain because of a natural pump (P-glycoprotein) that kicks it out. Studies show less than 2% risk of worsening motor symptoms. The problem? It’s not available as an injection in the U.S. and requires special approval from the FDA.
Cyclizine works differently. It blocks histamine receptors, not dopamine. The GGC Medicines Update (2023) rates its risk at just 5-10%. One patient on the Parkinson’s NSW Forum switched from metoclopramide to cyclizine and said, “The difference was night and day-no more freezing episodes.”
Ondansetron is a middle ground. It targets serotonin receptors, not dopamine. It’s about 15-20% risky, mostly because it’s less effective for some types of nausea linked to Parkinson’s. But it’s widely available and often used when domperidone isn’t an option.
The Levodopa Nausea Trap
Here’s the cruel twist: the very drug that keeps you moving-levodopa-is the main cause of your nausea. That means you’re stuck. Treat the nausea, and you risk making Parkinson’s worse. Don’t treat it, and you might stop taking your meds altogether.That’s why non-drug options come first. The Parkinson’s Foundation recommends:
- Ginger (1 gram daily, as capsules or tea)
- Small, frequent meals instead of large ones
- Staying hydrated with water or electrolyte drinks
- Avoiding greasy or spicy foods
If those don’t work, try domperidone. If it’s not available, cyclizine is next. Ondansetron is third. And only after all else fails-and with a neurologist’s approval-might levomepromazine be considered. Even then, start low: 6.25 mg twice a day, max 25 mg daily.

What Doctors Still Get Wrong
A 2022 study in the Journal of Parkinson’s Disease found only 37% of ER doctors knew metoclopramide was dangerous for Parkinson’s patients. That’s terrifying. Many patients are given these drugs without anyone checking their medication list.One patient shared on Parkinson’s UK’s forum that she was given prochlorperazine in the ER for vomiting. Within hours, she couldn’t walk. She spent five days in the hospital. Her neurologist later said, “That could’ve been avoided if they’d asked about your Parkinson’s.”
That’s why the Movement Disorder Society now requires a special note on every prescription: “Parkinson’s disease: verify antiemetic safety.” Some hospitals have started using electronic alerts, but many still rely on paper charts.
Even worse, some doctors think metoclopramide is “safe” because it doesn’t cause Parkinsonism in everyone. But that’s misleading. Dr. Alberto Espay of the University of Cincinnati says, “The single most common medication error we see in Parkinson’s patients is the inappropriate prescription of metoclopramide for nausea.”
What’s Changing for the Better
Good news: things are improving. The Parkinson’s Foundation’s 2023 Quality Improvement Initiative trained over 1,200 providers. In hospitals that participated, inappropriate antiemetic prescriptions dropped by 55%.New drugs are coming too. Aprepitant (Emend), which blocks a different nausea pathway (neurokinin-1), showed 92% effectiveness in a 2023 trial with zero motor side effects. The Michael J. Fox Foundation is funding a $1.2 million project to develop a new peripheral serotonin modulator-designed specifically for Parkinson’s patients, with no brain penetration.
And the American Geriatrics Society now lists metoclopramide as “potentially inappropriate” for Parkinson’s patients in its 2023 Beers Criteria. That’s a big deal. It means geriatricians, ER docs, and even pharmacists are now being taught this isn’t just a neurology issue-it’s a safety issue across all specialties.
What You Can Do Today
If you have Parkinson’s:- Carry a wallet card listing your medications and the antiemetics to avoid. The APDA has distributed over 250,000 of these since 2018. Patients with the card report 40% fewer bad prescriptions.
- Always tell every doctor, nurse, or pharmacist you see: “I have Parkinson’s. Do not give me metoclopramide, prochlorperazine, or haloperidol.”
- Ask for domperidone or cyclizine instead. If they say it’s not available, ask for a referral to a neurologist or movement disorder specialist.
- Keep a nausea diary: what you ate, when you felt sick, what meds you took. This helps your doctor spot patterns and adjust treatment.
- Never stop levodopa because of nausea. Talk to your neurologist about adjusting the dose or adding a safer antiemetic.
The bottom line: nausea in Parkinson’s is treatable-but not with the usual go-to drugs. The right antiemetic won’t just make you feel better. It can keep you moving, independent, and out of the hospital.
Can I take Zofran (ondansetron) if I have Parkinson’s?
Yes, ondansetron is generally safe for Parkinson’s patients because it doesn’t block dopamine receptors. It targets serotonin instead. However, it’s not always as effective for nausea caused by levodopa, and some patients report it doesn’t work well for motion-related nausea. Use it if safer options like domperidone or cyclizine aren’t available, but don’t expect it to work for everyone.
Is domperidone available in the U.S.?
Domperidone isn’t FDA-approved for general use in the U.S. due to a black box warning about heart rhythm risks at high doses. But it’s available through a special FDA program called an Investigational New Drug (IND) application. Many neurologists can help you get it. It’s often prescribed off-label for Parkinson’s patients because it’s the safest antiemetic option for brain dopamine pathways.
Why is metoclopramide still prescribed if it’s so dangerous?
It’s cheap, widely available, and works fast for nausea in the general population. Many doctors don’t know it’s risky for Parkinson’s patients, especially in emergency rooms or for older adults. Studies show over 60% of ER physicians don’t recognize the danger. That’s why patient advocacy and clear communication are critical-you have to speak up.
Can I use ginger instead of medication for nausea?
Yes, ginger is a proven, safe first-line option. Take 1 gram daily in capsule form or as tea. Studies show it reduces nausea in Parkinson’s patients without affecting dopamine. It’s not as strong as domperidone, but it’s risk-free and can be used alongside other treatments. Try it before jumping to medication.
What should I do if I was given metoclopramide and my symptoms got worse?
Stop taking it immediately. Contact your neurologist or Parkinson’s specialist. If symptoms are severe-like sudden inability to walk, swallowing trouble, or confusion-go to the ER and tell them you have Parkinson’s and were given a dopamine-blocking antiemetic. Bring your medication list. Most symptoms improve within days after stopping the drug, but recovery can take up to 3 weeks. Document everything: dates, doses, symptoms. This helps prevent future mistakes.
Next Steps for Patients and Caregivers
If you’re managing Parkinson’s:- Make a list of all your medications and share it with every provider-even the dentist.
- Ask your neurologist to write a letter to your primary care doctor and ER team listing safe antiemetics.
- Download the APDA’s Medications to Avoid wallet card and keep it in your wallet or phone.
- If you’re a caregiver, learn the names of the dangerous drugs: metoclopramide, prochlorperazine, haloperidol, chlorpromazine. Say no to them.
- Join a Parkinson’s support group. Real stories from others who’ve been through this can save your life.
There’s no excuse for another Parkinson’s patient to be harmed by a preventable drug interaction. Knowledge is power-and in this case, it’s mobility, dignity, and safety.



Just had my doc try to push me on metoclopramide last month for nausea after chemo. Thank god I read this thread first. Told him flat out: 'I don't wanna turn into a statue.' He actually listened. Gave me cyclizine instead. Still works, no brain freeze. Small wins, right?
December 10Paul Dixon