Personalized Antiplatelet Therapy Calculator
How This Tool Works
Based on clinical evidence, this tool estimates your bleeding risk and ischemic event risk for each antiplatelet drug. It considers your age, weight, medical history, and other factors mentioned in the article. This is for educational purposes only and should not replace medical advice.
Important Disclaimer
This tool is for educational purposes only and does not replace professional medical advice. Always consult your doctor before making any changes to your medication.
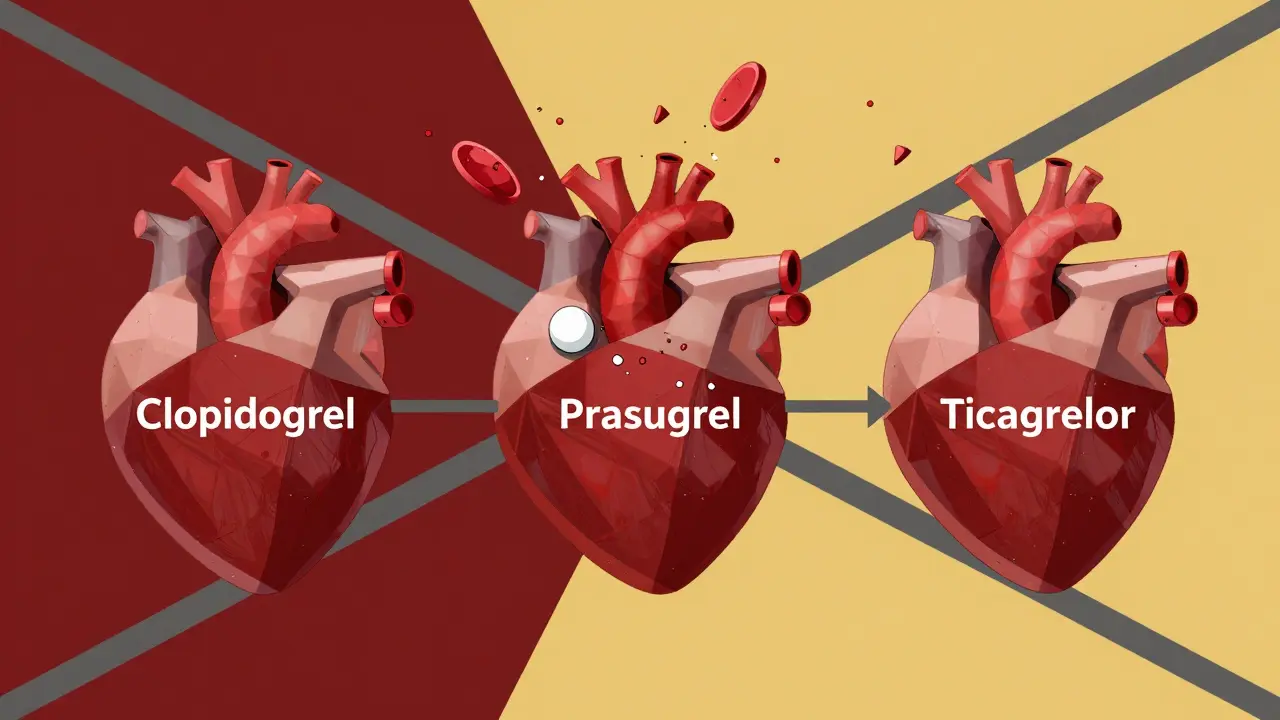
When you’ve had a heart attack or stent placed, your doctor doesn’t just hand you a pill and say "good luck." They pick one of three powerful antiplatelet drugs-clopidogrel, prasugrel, or ticagrelor-each with different risks, benefits, and side effects. These aren’t just generic blood thinners. They work differently, hit your body differently, and can change your daily life in ways you might not expect. Choosing the wrong one isn’t just about cost-it’s about whether you’ll bleed too much, struggle to breathe, or end up back in the hospital because the drug didn’t work.
How These Drugs Actually Work
All three drugs block the P2Y12 receptor on platelets, the tiny blood cells that clump together to form clots. That’s good when you’re trying to prevent a second heart attack. But it’s dangerous when you cut your finger or fall down the stairs. Clopidogrel and prasugrel are thienopyridines-they need your liver to turn them into active forms. Ticagrelor is different. It works right away, doesn’t need liver conversion, and binds reversibly. That means its effects fade faster when you stop taking it.
This matters because if your liver can’t process clopidogrel properly-about 30% of people, especially those with certain genes-you get little to no protection. Prasugrel is more reliable in these cases. Ticagrelor? It doesn’t care about your liver genes. It just works.
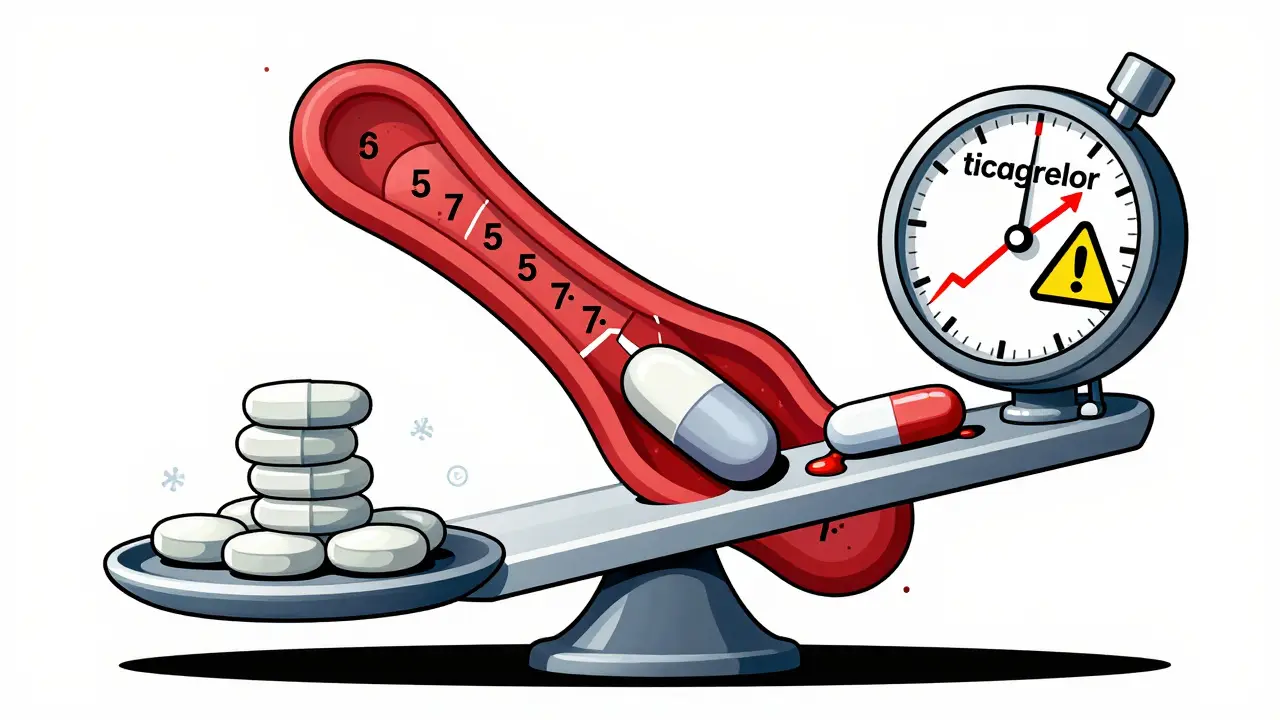
Bleeding: The Big Risk
The biggest danger with all three is bleeding. Not just a nosebleed. Major bleeding-like bleeding into your brain, stomach, or intestines-that can kill you.
Prasugrel has the highest bleeding risk. In the TRITON-TIMI 38 trial, people on prasugrel had 2.4% major bleeding vs. 1.8% on clopidogrel. That might sound small, but in a population of 10,000 patients, that’s 60 extra people with life-threatening bleeds. The risk jumps even higher if you’re over 75 or weigh less than 60 kg. Many cardiologists avoid prasugrel in older patients entirely. One doctor told me he saw an 80-year-old’s hemoglobin drop from 12 to 8 g/dL in two weeks on prasugrel. That’s a blood transfusion waiting to happen.
Ticagrelor isn’t far behind. The PLATO trial showed a slight increase in major bleeding (2.6% vs. 2.3%) compared to clopidogrel. But here’s the twist: ticagrelor reduced heart attack deaths by 21%. So you trade a little more bleeding for fewer deaths. That’s why guidelines now prefer ticagrelor for most ACS patients.
Clopidogrel is the safest in terms of bleeding, but only if it works. If you’re a poor metabolizer, you’re not protected at all. That means you could have a heart attack while thinking you’re safe.
Ticagrelor’s Weird Side Effect: Can’t Breathe
If you’ve never heard of ticagrelor causing shortness of breath, you’re not alone. But it happens in 14-16% of people. That’s 1 in 7 patients. It’s not anxiety. It’s not asthma. It’s a direct drug effect.
Patients describe it as "feeling like I’m drowning," "like a weight on my chest," or "can’t catch my breath even when sitting still." It usually starts within days. In clinical trials, it was 1.7 times more common than with clopidogrel. And here’s the catch: it’s not dangerous on its own. No lung damage. No heart strain. But it’s so uncomfortable that 15-20% of people stop taking it.
Doctors now tell patients upfront: "You might feel like you’re suffocating. It’s the drug. It’s not your heart. It usually gets better after a few weeks." If you’re counseled, 60-70% stick with it. Without that talk? Half quit.
Other Side Effects You Won’t Hear About
Ticagrelor can also cause brief pauses in your heartbeat-ventricular pauses. About 3% of people get them. They’re usually harmless, but if you have a pacemaker or existing heart rhythm issues, your doctor needs to know.
Prasugrel has a black box warning from the FDA: don’t use it if you’ve had a stroke or TIA. It increases fatal bleeding in those patients. And if you’re over 75? The risk is so high many hospitals won’t even prescribe it.
Clopidogrel’s biggest issue isn’t side effects-it’s failure. If you’re a CYP2C19 poor metabolizer, you’re not getting the full benefit. That’s why some hospitals test for this gene before prescribing. But the test costs $200-$300, and guidelines say it’s not worth it for everyone. Only for high-risk cases-like someone with diabetes and a stent who’s already had a clot.
Dosing and Timing Matter More Than You Think
Prasugrel and clopidogrel are irreversible-they permanently disable platelets. That means once you take them, your platelets are out of commission for their entire life cycle (7-10 days). Ticagrelor is reversible. It wears off in 3-5 days.
This is critical if you need surgery. If you’re on prasugrel, you need to stop 7 days before surgery. Clopidogrel? 5 days. Ticagrelor? Just 3 days. That’s a big deal if you’re scheduled for an emergency procedure. Ticagrelor gives you more flexibility.
Also, ticagrelor is taken twice daily. Prasugrel and clopidogrel are once daily. That affects adherence. One study found 21% more people quit ticagrelor because of side effects or dosing hassle.
Cost and Accessibility
Clopidogrel costs about $10 a month as a generic. Prasugrel and ticagrelor? Around $300-$400. Insurance often covers them, but copays can be steep. In real-world use, 60% of prescriptions are still for clopidogrel-not because it’s better, but because it’s cheap.
But here’s the trade-off: if clopidogrel fails because of your genes, you’re at higher risk of another heart attack. That’s not just a medical cost-it’s lost work, ER visits, possible disability.
What Doctors Actually Choose
A 2022 survey of over 1,200 cardiologists showed:
- 42% prefer ticagrelor for ACS patients
- 35% still use clopidogrel for cost reasons
- 23% pick prasugrel only for high-risk PCI cases
Why? Ticagrelor works better, especially for preventing death. Prasugrel is strong but too risky for most. Clopidogrel is the fallback-cheap, familiar, but unreliable in a third of patients.
For someone under 75 with no history of stroke and a high risk of another clot? Prasugrel might be the best bet. For someone older, with other health issues, or who needs flexibility for possible surgery? Ticagrelor. For someone on a tight budget with no genetic risk? Clopidogrel can still work.
New Developments: Lower Doses and Better Choices
In 2023, the FDA approved a lower dose of ticagrelor-30 mg twice daily-for long-term use after the first year. The MATTERHORN trial showed this reduced bleeding by 25% without losing protection against heart attacks. Now, many doctors start patients on 90 mg twice daily for the first 12 months, then drop to 30 mg. This is a game-changer for people who can’t tolerate the higher dose.
Guidelines now recommend tailoring treatment: high ischemic risk? Stay on ticagrelor or prasugrel for 6-12 months. High bleeding risk? Switch to aspirin alone or low-dose ticagrelor after 12 months.
Future drugs like selatogrel (a subcutaneous option) are in trials. They might let you control your antiplatelet effect like a dimmer switch-turn it up for high risk, turn it down for surgery. But that’s still years away.
What You Should Do
If you’re on one of these drugs:
- Don’t stop it without talking to your doctor-even if you feel fine.
- If you’re on ticagrelor and suddenly can’t breathe, call your doctor. Don’t assume it’s anxiety.
- If you’re on clopidogrel and had a clot despite taking it, ask about genetic testing.
- If you’re scheduled for surgery, tell your surgeon what you’re taking and when you last took it.
- Never mix these with NSAIDs like ibuprofen or naproxen. That doubles your bleeding risk.
There’s no one-size-fits-all here. Your age, weight, genetics, risk of clotting, risk of bleeding, cost, and lifestyle all matter. Your doctor should walk you through this-not just hand you a prescription and move on.
Can I take clopidogrel if I have a history of stroke?
Yes, clopidogrel is generally safe after a stroke. But prasugrel is not. The FDA has a black box warning against prasugrel in patients with prior stroke or TIA because it significantly increases the risk of fatal bleeding in the brain. Ticagrelor is an option, but only if your doctor determines the benefit outweighs the bleeding risk. Always disclose your full medical history before starting any antiplatelet drug.
Why does ticagrelor cause shortness of breath?
The exact reason isn’t fully understood, but ticagrelor blocks a specific receptor (adenosine receptor A2A) that helps regulate breathing. This causes a sensation of breathlessness, not because your lungs are damaged, but because your brain senses a change in oxygen signaling. It’s not dangerous, but it’s very uncomfortable. Most patients adapt within 2-4 weeks. If you’re told this is "just anxiety," ask for a second opinion.
Is prasugrel better than ticagrelor for someone with a stent?
For high-risk patients under 75 with no prior stroke, prasugrel may offer slightly better protection against stent clots and heart attacks. But it comes with a higher bleeding risk. Ticagrelor is nearly as effective and safer for bleeding. Most guidelines now favor ticagrelor because the survival benefit is clearer and the side effects are more manageable. Your doctor should weigh your personal risk of clotting versus bleeding-not just pick the "strongest" drug.
How long do I need to take these drugs after a stent?
For most people, dual antiplatelet therapy (aspirin + one of these drugs) lasts 6-12 months after a stent. After that, you usually switch to aspirin alone. But if you’re at high risk for another clot-like if you have diabetes, kidney disease, or had a large heart attack-your doctor may extend ticagrelor or prasugrel beyond a year, sometimes at a lower dose (like 30 mg of ticagrelor). Never stop on your own.
Can I switch from clopidogrel to ticagrelor if it’s not working?
Yes, and it’s often recommended if you’ve had a clot despite taking clopidogrel. This is called "therapeutic failure," and it’s common in people with CYP2C19 gene variants. Switching to ticagrelor or prasugrel can cut your risk of another event by nearly half. Talk to your cardiologist about a platelet function test or genetic test to confirm the issue before switching.
If you’re on one of these drugs and feel something’s off-whether it’s trouble breathing, unusual bruising, or just a gut feeling-don’t ignore it. These aren’t ordinary pills. They’re powerful tools that demand attention. The right one can save your life. The wrong one? It might cost you more than you think.


Ticagrelor makes me feel like I’m underwater. Not anxiety. Not asthma. Just... can’t breathe. I quit after 3 days.
January 14Lance Nickie