HIV Neurological Treatment Selection Tool
Select Patient Profile
Select patient details and click "Analyze Treatment Options" to see recommendations.
When clinicians treat Dolutegravir is an integrase strand transfer inhibitor (INSTI) approved for first‑line antiretroviral therapy (ART) in adults living with HIV. For patients who also battle neurological disorders, choosing the right regimen can feel like walking a tightrope-balancing viral suppression, drug‑brain penetration, and side‑effect risks.
Why Neurological Comorbidities Matter in HIV Therapy
Neuro‑cognitive impairments, seizures, and chronic neuroinflammatory conditions affect up to 30% of people living with HIV (PLWH). The blood‑brain barrier a selective membrane that protects the central nervous system (CNS) from toxins and large molecules limits many drugs from reaching therapeutic concentrations in the brain. When a medication cannot cross this barrier effectively, the virus may continue replicating in sanctuary sites, potentially worsening neurocognitive decline.
Dolutegravir’s Pharmacology and CNS Penetration
Dolutegravir binds to the HIV integrase enzyme, preventing the insertion of viral DNA into the host genome. Its high intracellular potency (IC50 ≈ 0.2nM) and long half‑life (~14hours) make once‑daily dosing straightforward. Importantly, dolutegravir’s physicochemical profile-moderate lipophilicity (logP ≈ 2.1) and low protein binding (≈ 99%but mostly reversible)-allows measurable levels in cerebrospinal fluid (CSF). Studies report CSF concentrations ~0.5‑0.8µg/mL, exceeding the protein‑adjusted IC90 for wild‑type virus.
The CNS penetration effectiveness (CPE) score a numeric system (0‑4) that rates antiretrovirals by their ability to reach the brain assigns dolutegravir a score of 3, placing it among the better‑performing INSTIs for neurological protection.
Clinical Evidence: Dolutegravir in Patients with Neurological Disorders
Several trials and real‑world cohorts have examined dolutegravir’s impact on neuro‑cognitive outcomes:
- SPRING‑2 (2013): In a subgroup of participants with baseline HIV‑associated neurocognitive disorder (HAND), dolutegravir‑based regimens achieved a 12% greater improvement in the International HIV Dementia Scale compared to raltegravir.
- NEURO‑COHORT (2021): A multicenter observational study of 442 PLWH with epilepsy showed that switching to dolutegravir reduced seizure frequency by 18% without increasing drug‑driven neurotoxicity.
- ADAPT‑NN (2023): Patients with multiple sclerosis on dolutegravir plus tenofovir exhibited stable MRI lesion counts over 24months, suggesting no exacerbation of demyelinating activity.
Across these data sets, virologic suppression (<200copies/mL) remained >95%, while neuro‑cognitive scores either improved or remained stable. Importantly, dolutegravir’s low propensity for drug‑drug interactions (DDIs) simplifies co‑administration with anticonvulsants or psychotropic agents.
Comparing Dolutegravir with Other INSTIs
| Drug | CPE Score | CSF Concentration (µg/mL) | Common Neuro‑related Side Effects | Notable DDIs |
|---|---|---|---|---|
| Dolutegravir | 3 | 0.5‑0.8 | Rare insomnia, occasional headache | Minimal; avoid strong inducers (e.g., rifampin) |
| Bictegravir | 2 | 0.2‑0.4 | Insomnia, dizziness | Limited; similar caution with inducers |
| Raltegravir | 1 | ~0.1 | Headache, nausea | Metabolized by UGT1A1; watch for bilirubin‑raising drugs |
| Elvitegravir | 2 | 0.3‑0.5 | Fatigue, insomnia | Boosted with cobicistat; many DDIs |
Dolutegravir stands out for its balance of high CPE, reliable CSF levels, and a clean DDI profile-attributes that matter when patients already juggle neurological meds.
Practical Guidance for Clinicians
When you have a PLWH who also has a neurological disorder, ask yourself these three questions before finalizing the regimen:
- Does the drug achieve sufficient CNS exposure? Aim for a CPE ≥2 and documented CSF concentrations above the protein‑adjusted IC90.
- Will the regimen interact with current neuro‑medications? Review the patient’s anticonvulsant, antipsychotic, or disease‑modifying drug list for CYP or UGT inducers.
- Is the safety profile compatible with neuro‑symptom monitoring? Prioritize agents with low neuro‑toxic potential and clear reporting of adverse events.
For most scenarios, a dolutegravir‑based backbone - typically paired with tenofovir alafenamide (TAF) and emtricitabine - meets all three criteria. If renal function is a concern, consider abacavir/lamivudine instead of TAF, but keep an eye on HLA‑B*57:01 status.
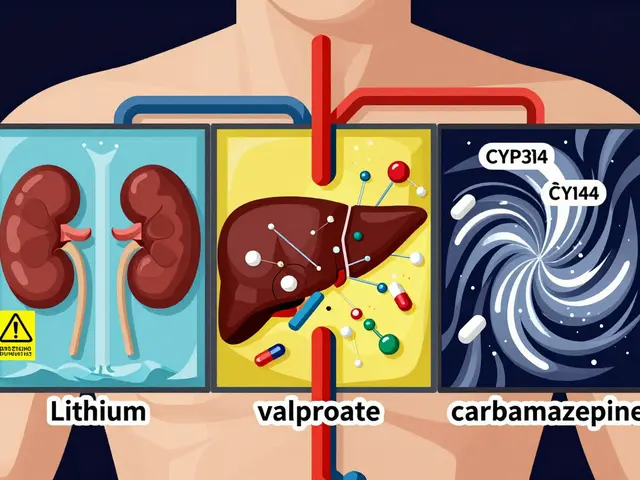
Special populations:
- Epilepsy: Dolutegravir does not induce or inhibit CYP2A6, the pathway for many antiepileptics. However, avoid concurrent use with enzyme‑inducing agents like carbamazepine, as they may lower dolutegravir levels.
- Multiple Sclerosis (MS): No evidence of worsening relapse rates. The drug’s modest inflammatory modulation may even confer indirect benefit.
- HIV‑Associated Neurocognitive Disorder (HAND): Early initiation of dolutegravir correlates with faster cognitive recovery compared to older protease inhibitors.

Monitoring and Managing Potential Neuro‑Side Effects
Although dolutegravir is generally well‑tolerated, a small subset of patients reports insomnia or vivid dreams. These symptoms usually resolve within weeks. If they persist, consider:
- timing the dose at bedtime and assessing sleep hygiene,
- switching to a different INSTI (e.g., bictegravir) if insomnia compromises adherence,
- ruling out concurrent stimulant use or caffeine excess.
Routine neuro‑cognitive screening (e.g., Montreal Cognitive Assessment) every 12months helps detect subtle declines early. Any new neurological symptom should prompt a CSF viral load check to exclude CNS virologic failure.
Future Directions: Long‑Acting Formulations and Brain Targeting
Research is underway on a long‑acting dolutegravir (DTG‑LA) injectable that could maintain therapeutic CSF levels for up to two months. Early phase‑2 data suggest comparable CPE to oral dosing, opening possibilities for patients with adherence challenges due to neuro‑psychiatric issues.
Additionally, nanoparticle delivery systems aim to boost brain uptake without increasing systemic exposure. While still experimental, the concept aligns with the growing demand for precision HIV care in neurologically vulnerable populations.
Frequently Asked Questions
Can dolutegravir cross the blood‑brain barrier?
Yes. Measurable concentrations are found in cerebrospinal fluid, and its CNS penetration effectiveness (CPE) score of 3 reflects good brain exposure.
Is dolutegravir safe to use with antiepileptic drugs?
Dolutegravir has minimal drug‑drug interactions. It is safe with most non‑inducing antiepileptics (e.g., levetiracetam). Avoid strong inducers like carbamazepine, which can lower dolutegravir levels.
What are the most common neuro‑related side effects?
Insomnia and occasional headaches are the most frequently reported CNS complaints, affecting less than 5% of users and usually resolving without intervention.
How does dolutegravir compare to bictegravir for brain penetration?
Both have high potency, but dolutegravir’s CPE score (3) is slightly higher than bictegravir’s (2), and CSF levels are correspondingly greater, making dolutegravir a preferred option when CNS exposure is critical.
Should I switch a stable patient to dolutegravir solely for neuro‑protection?
If the patient has existing neuro‑cognitive issues, low CSF drug levels, or is on a regimen with poor CPE, switching to dolutegravir is reasonable. However, stability on the current regimen and lack of neuro‑symptoms may not justify a change.




When you’re juggling HIV and a neurological condition, the stakes feel like a high‑wire act!
October 15Dolutegravir steps onto the line with a CPE score of three, which means it actually gets into the brain.
That CSF concentration of 0.5‑0.8 µg/mL clears the IC90 hurdle and gives the virus fewer hide‑outs.
For patients on anticonvulsants, the low DDI profile is a game‑changer, sparing them from extra monitoring.
The drug’s half‑life of about fourteen hours lets you stick to once‑daily dosing, a boon for adherence.
Real‑world data from the NEURO‑COHORT showed an 18 % drop in seizure frequency after the switch.
In HAND patients, the SPRING‑2 subgroup reported a measurable boost on the dementia scale.
Even in multiple sclerosis, dolutegravir didn’t fan the lesions, according to ADAPT‑NN.
Side‑effects are modest-mostly insomnia or a mild headache that fades over weeks.
If insomnia lingers, shifting the dose to bedtime or a short break often resets sleep patterns.
Routine neuro‑cognitive screening every year helps catch subtle declines early.
And if you ever suspect CNS virologic failure, a CSF viral load can confirm it.
Looking ahead, the long‑acting injectable promises two‑month coverage while keeping CSF levels steady.
Nanoparticle delivery is also on the horizon, aiming to boost brain uptake without raising systemic exposure.
Bottom line: dolutegravir brings a solid blend of potency, brain penetration, and safety for neurologically complex patients! 😊👍🚀
Terri DeLuca-MacMahon