Chemotherapy Nausea Management Planner
Your Personalized Nausea Management Plan
Dealing with chemotherapy nausea can feel like an endless battle, but the good news is there are practical steps that actually work. Below you’ll find a mix of medical, dietary, and lifestyle strategies that can keep the queasy feeling under control without sacrificing your energy or overall health.
Key Takeaways
- Start a food‑and‑fluid routine 30minutes before treatment.
- Try proven natural aids such as ginger, acupressure, and peppermint.
- Know the main classes of anti‑emetic medication and when each is appropriate.
- Track triggers and patterns; small adjustments can make a big difference.
- Seek medical advice if nausea persists beyond 48hours or affects weight.
Understanding Chemotherapy‑Induced Nausea
Chemotherapy‑Induced Nausea is a side effect that occurs when cytotoxic drugs irritate the stomach lining or stimulate the brain’s vomiting center. It usually peaks within the first 24hours after infusion but can linger for several days, especially with highly emetogenic regimens. Knowing that the body’s response is a mix of chemical signals and gut irritation helps you target the right interventions.
Daily Lifestyle Strategies
Simple habits can dramatically lower the intensity of nausea.
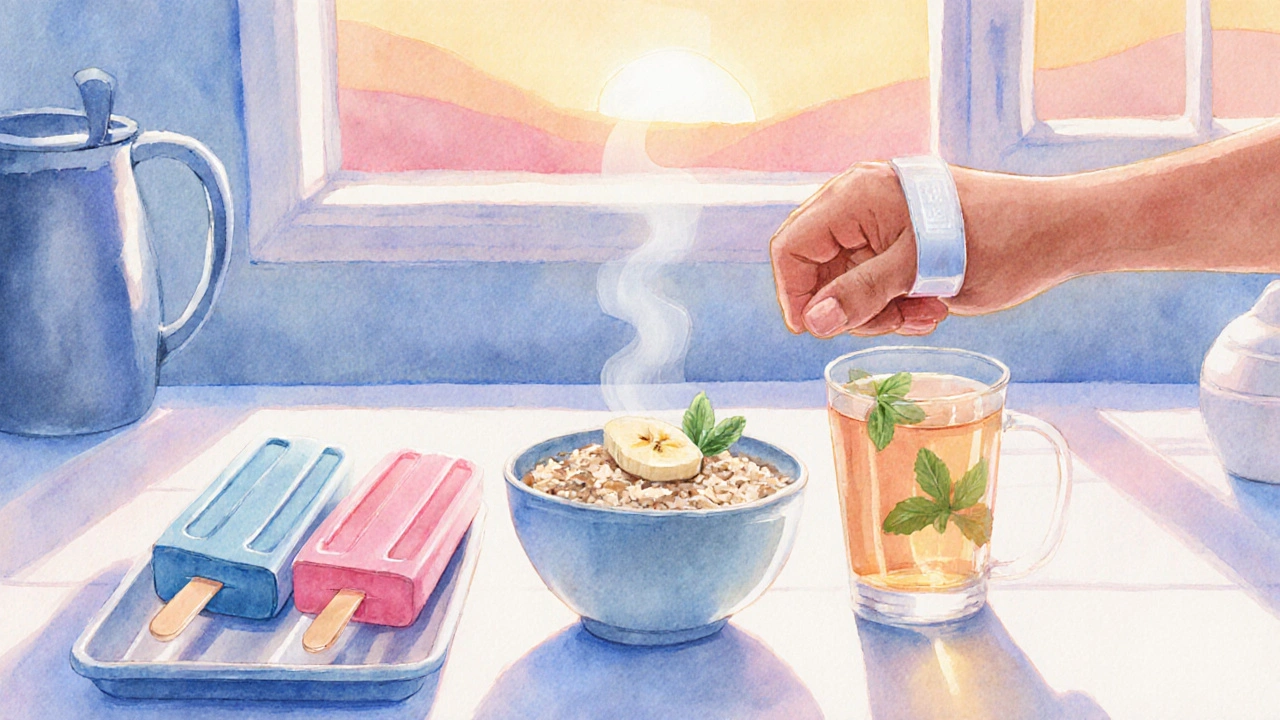
- Hydration timing: Sip clear fluids (water, diluted juice, herbal tea) at least 30minutes before chemo and continue small sips afterward. Warm drinks tend to settle the stomach better than cold ones.
- Rest and positioning: Rest in a semi‑upright position for the first hour post‑treatment. Lying flat can increase pressure on the stomach and worsen queasiness.
- Stress reduction: Deep‑breathing exercises, guided imagery, or short meditation sessions (5‑10minutes) lower cortisol, which can heighten nausea sensations.
Dietary Adjustments That Work
What you eat matters as much as what you avoid.
- Small, frequent meals: Aim for 5‑6 mini‑meals spread over the day instead of three large ones. A light snack 30minutes before chemo (e.g., plain toast with apple sauce) can provide a protective coating for the stomach.
- Ginger in any form-fresh, tea, capsules-has been shown in multiple clinical trials to cut nausea severity by up to 40% when taken 15minutes before treatment.
- Low‑fat, bland foods: Crackers, rice, bananas, and oatmeal are easy on the digestive tract. Avoid greasy, fried, or heavily seasoned dishes that can trigger reflux.
- Cold foods: Popsicles, chilled fruit, or yogurt are often better tolerated than hot soups during a nausea episode.
Physical Complementary Techniques
Non‑pharmacologic methods can be powerful when used consistently.
- Acupressure wrist bands (Nei‑Guan point) applied 30minutes before chemo have reduced nausea scores in several studies. Press the band firmly for a few seconds every hour.
- Peppermint aromatherapy: Inhaling peppermint oil or sipping peppermint tea can relax the smooth muscles of the GI tract.
- Progressive muscle relaxation: Tense‑then‑relax each muscle group, starting at the feet and moving upward, for 10‑15minutes. This technique lowers sympathetic nervous activity that can amplify nausea.
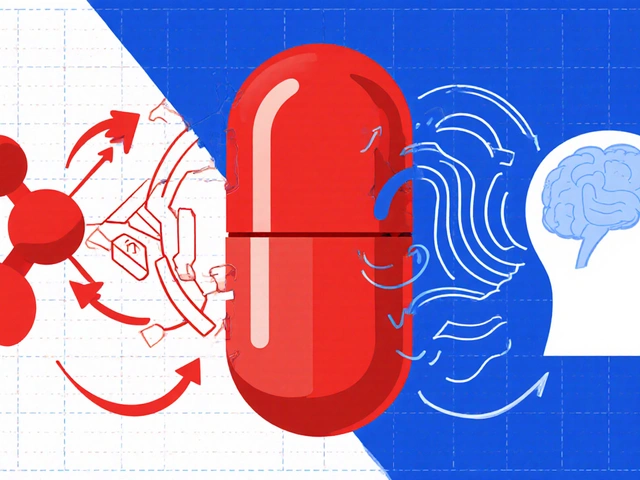
Medication Options and How to Choose
When lifestyle tweaks aren’t enough, anti‑emetic drugs become essential. Below is a quick comparison of the three major classes used alongside chemotherapy.
| Class | Common Drug | Mechanism | Typical Side Effects | Onset |
|---|---|---|---|---|
| 5‑HT3 Antagonists | Ondansetron | Blocks serotonin receptors in the gut and brain | Headache, constipation | 15‑30min (IV), 1‑2h (oral) |
| NK1 Receptor Antagonists | Aprepitant | Inhibits substance P binding in the brain | Fatigue, dizziness | 2‑3h (oral) |
| Corticosteroids | Dexamethasone | Reduces inflammation and interacts with neurotransmitter pathways | Increased appetite, insomnia | 30‑60min (IV) |
For highly emetogenic regimens, doctors often prescribe a combination of a 5‑HT3 antagonist, an NK1 blocker, and a low‑dose corticosteroid. If you’re on a moderate‑risk protocol, a single 5‑HT3 drug plus a short course of dexamethasone may suffice.
Always discuss dosage timing with your oncology team. Taking the anti‑emetic 30minutes before infusion maximizes its preventive effect.

When to Seek Professional Help
Even the best home plan can reach its limit. Contact your treatment center if you experience any of the following:
- Persistent vomiting for more than 24hours.
- Weight loss exceeding 5% of body weight.
- Severe dehydration (dry mouth, dizziness, dark urine).
- New‑onset severe abdominal pain or fever.
Prompt medical attention can prevent complications such as electrolyte imbalance and can lead to adjustments in your anti‑emetic regimen.
Quick Checklist for the Day of Treatment
- Eat a light, bland snack 30minutes before arrival.
- Take prescribed anti‑emetic on schedule (usually an hour prior).
- Drink 8‑10oz of water or clear juice; avoid carbonated drinks.
- Apply acupressure wrist band before infusion and keep it on for the first 4hours.
- Carry ginger chews or peppermint tea for after‑treatment relief.
- Rest in a semi‑upright position for at least an hour post‑infusion.
- Log any nausea episodes, foods, or activities that seemed to help or worsen symptoms.
Frequently Asked Questions
Can I take ginger supplements if I’m already on anti‑emetic drugs?
Yes. Ginger is generally safe and works through a different pathway (gastric motility) than most prescription anti‑emetics. However, discuss the dose with your oncologist, especially if you’re on blood thinners.
Is it okay to skip meals during chemo to avoid nausea?
Skipping meals can actually worsen nausea because an empty stomach is more sensitive. Aim for small, frequent bites that are easy to digest.
How long should I keep using acupressure bands?
Most patients find relief for the first 24‑48hours post‑chemo. If nausea persists beyond that, consider other interventions and talk to your care team.
Are there any foods I should completely avoid?
Strongly fried, spicy, or high‑fat dishes often trigger reflux and nausea. Also, very sweet desserts can cause blood‑sugar spikes that make you feel queasy.
When is it necessary to adjust my medication?
If nausea occurs despite taking your anti‑emetic as prescribed, or if side effects become intolerable, contact your oncologist. Dose adjustments or adding a different class (e.g., NK1 antagonist) are common solutions.



One must contemplate the interplay between physiological mechanisms and patient agency when confronting chemotherapy‑induced nausea. A structured routine, as outlined, provides a scaffold upon which individuals can assert control. The emphasis on timing, hydration, and dietary selection reflects a nuanced understanding of gastro‑intestinal dynamics. Moreover, integrating evidence‑based complementary techniques, such as acupressure, showcases an interdisciplinary approach. Ultimately, this synthesis aligns with a philosophy of empowered self‑management.
October 8Samantha Dean