When you pick up a prescription, you might not think about the legal maze behind whether you get the brand-name drug or a cheaper generic. But in the United States, the answer depends entirely on which state you’re in. One state may require your pharmacist to swap the brand for a generic unless you say no. Another might demand your written permission. And in a few, certain drugs can’t be switched at all-even if the FDA says they’re identical.
Why State Laws on Generic Substitution Even Exist
The push for generic drug substitution started in the 1970s. The goal was simple: cut drug costs without sacrificing safety. The federal Hatch-Waxman Act of 1984 created a clear path for the FDA to approve generics that are chemically identical to brand-name drugs. But the law didn’t force pharmacies to switch. That’s where states stepped in. Today, every state has its own rules. Why? Because healthcare delivery is managed locally. Legislatures wanted control over how pharmacists handle prescriptions. The idea was to save money-billions of it. From 2009 to 2019, generic drugs saved the U.S. healthcare system $1.7 trillion. But with savings came concerns: What if a patient reacts differently to a generic? What if the drug has a narrow therapeutic index-where even tiny differences can cause harm? That’s why rules got complicated. Some states prioritize cost savings. Others prioritize control. And the result? A patchwork system that makes it hard for pharmacists, confusing for patients, and a headache for insurers.The Four Big Ways States Differ
Not all state laws are created equal. They vary in four key areas:- Whether substitution is mandatory or permissive - In 22 states, pharmacists must substitute a generic unless the doctor or patient says no. In the other 28 states and D.C., they can substitute-but only if they choose to.
- How patient consent works - In 32 states, consent is presumed. That means the pharmacist swaps the drug and tells you afterward. In 18 states, you must say yes before the switch happens.
- Notification requirements - Forty-one states require pharmacists to notify you after substitution, whether by phone, label, or in-person. The rest don’t.
- Legal protection for pharmacists - Thirty-seven states shield pharmacists from lawsuits if they follow the rules. Mississippi, for example, says pharmacists can’t be held liable if they substitute correctly. In states without this protection, pharmacists face more risk.
These differences aren’t just paperwork. They change how often generics are used. A 2018 study found that states with mandatory substitution had 12.3% higher generic fill rates for statins than states where substitution was optional. Presumed consent laws boosted substitution by 8.7% across multiple drug classes.
Narrow Therapeutic Index Drugs: The Big Exception
Not all drugs are treated the same. Some, called narrow therapeutic index (NTI) drugs, have a tiny window between an effective dose and a dangerous one. Warfarin (a blood thinner), levothyroxine (for thyroid conditions), and certain epilepsy medications fall into this category. The FDA says generics for these drugs are equivalent. But doctors and patients worry. The FDA’s own adverse event reports show over 140 cases between 2020 and 2022 where patients had problems after switching-mostly with levothyroxine and warfarin. Fifteen states have extra rules. Kentucky bans substitution for digitalis and antiepileptic drugs. Minnesota has documented cases where patients had seizures or bleeding after a generic switch, even though the drugs were labeled equivalent. In Hawaii, you need both the doctor’s and your own approval to switch an antiepileptic drug. Oklahoma goes even further: no substitution without written permission from the prescriber or the person paying for the drug.These rules exist because the stakes are high. A 0.1 mg change in levothyroxine can throw your metabolism off. A slight difference in warfarin can cause a stroke or internal bleeding. So while most generics are safe, these drugs trigger caution.

Biosimilars: The New Frontier
Biosimilars are the next wave of generic drugs-but they’re not like traditional generics. They’re made from living cells, not chemicals. That makes them harder to copy exactly. The FDA began approving them in 2015, and states had to catch up. As of 2023, 49 states and D.C. have laws for biosimilar substitution. But the rules vary wildly. Florida requires each pharmacy to create a formulary to ensure substitutions won’t harm patients. Iowa says to stick with the FDA’s Orange Book. Hawaii still requires both doctor and patient consent for biosimilars used to treat epilepsy. The biggest change? The FDA’s new “interchangeable” designation, introduced in 2020. It means a biosimilar can be swapped without the prescriber’s input-just like a regular generic. As of July 2023, 12 states updated their laws to match this. But 23 others are still reviewing their rules to align with the new FDA standards.What This Means for Pharmacists
For pharmacists, navigating these rules is exhausting. On average, they spend 12.7 minutes per prescription checking state laws, FDA lists, patient history, and prescriber notes. That’s time that could be spent counseling patients. The National Association of Boards of Pharmacy says 92% of states test pharmacists on substitution laws during licensing. But even certified pros get confused. A 2022 survey by the American Pharmacists Association found 78% of pharmacists struggle when filling prescriptions from out-of-state prescribers. One pharmacist in New York told Reddit users: “I have to ask every patient if they want the generic. In New Jersey, I just swap it unless they say no. Patients who live near the border get so confused-they think I’m making a mistake.” Technology is helping. Eighty-three percent of pharmacy systems now auto-check state laws. These tools reduce errors by 64%. But they’re not perfect. If a patient gets a prescription from a doctor in another state, the system might miss a local restriction.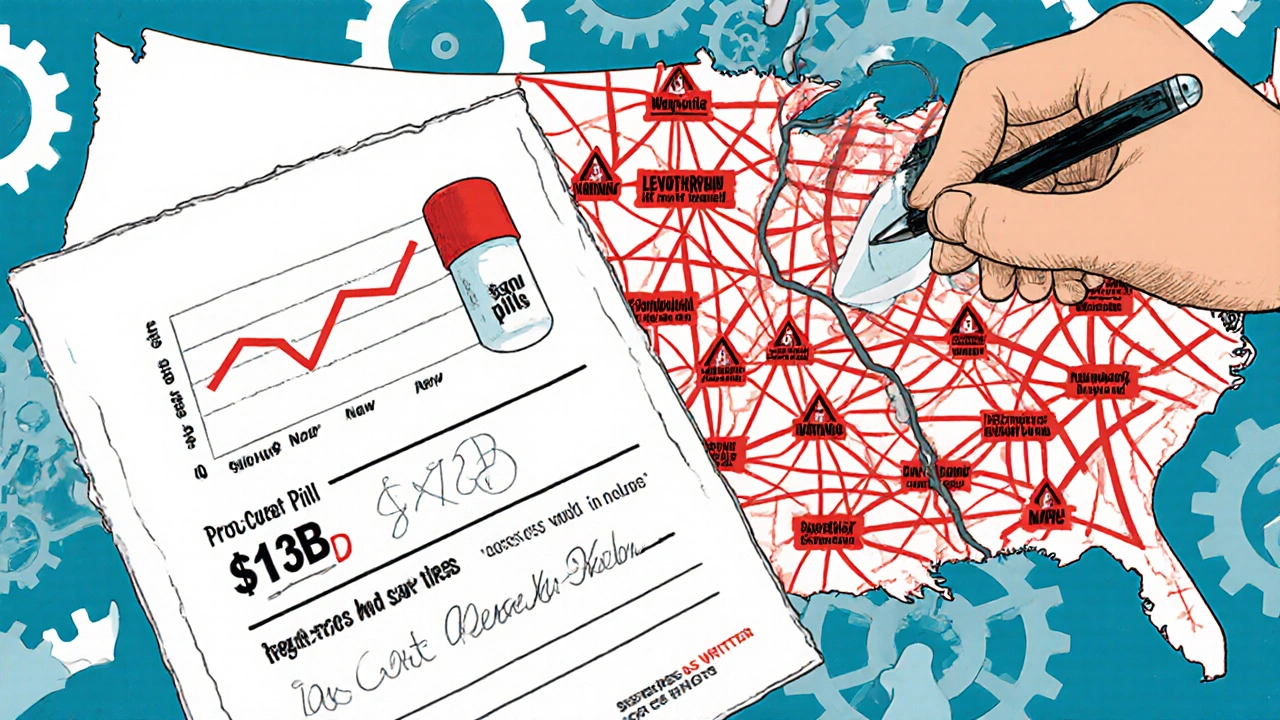
What Patients Experience
Most patients don’t know the rules. They just notice the price change. A 2022 survey of 1,200 independent pharmacists found that mandatory substitution laws cut prescription abandonment rates by 15.2%. That means fewer people skip their meds because they’re too expensive. In Texas, pharmacists saw fewer patients walk away from atorvastatin prescriptions after generics became automatic. But complaints exist. The FDA’s MedWatch system logged 217 reports between 2020 and 2022 about side effects after a switch. Most involved levothyroxine or warfarin. The Life Raft Group’s 2023 patient survey found 41% of cancer patients worried about substitution for NTI drugs. Nearly a third said their doctors told them to “dispense as written”-meaning no substitutions allowed. Patients near state borders face another issue. A person living in Pennsylvania but seeing a doctor in New Jersey might get different generics depending on where they fill the prescription. That inconsistency can trigger anxiety-and confusion.Costs, Savings, and the Future
Generic drugs now make up 92.5% of all prescriptions filled in the U.S. That’s up from 80% in 2010. The savings? $313 billion a year. States with mandatory substitution see generic fill rates of 94.1%. Permissive states? Just 88.3%. That gap matters. A 2018 study estimated mandatory laws save Medicaid programs $1.2 billion annually. But the system is unsustainable. With 50 different sets of rules, it’s inefficient. The Uniform Law Commission drafted a model bill in 2023 to harmonize biosimilar substitution laws across states. The Congressional Budget Office estimates that if all states aligned their rules, we could save an extra $8.7 billion by 2028. On the other side, patient advocates warn that too much standardization could hurt people with rare diseases. About 25-30 million Americans rely on NTI drugs. For them, a switch-even one deemed “equivalent”-could be dangerous.What You Can Do
You don’t need to memorize your state’s laws. But you can take control:- Ask your pharmacist: “Is this a generic? Can I get the brand instead?”
- If you’re on a critical drug like warfarin or levothyroxine, ask your doctor to write “Dispense as Written” on the prescription.
- If you notice side effects after a switch, report them to your doctor and the FDA’s MedWatch system.
- Know your state’s rules. A quick search for “[Your State] generic substitution law” will show you if consent is required.
Generic drugs save lives and money. But they’re not one-size-fits-all. The law reflects that. Understanding your rights-and your doctor’s-means you’re not just a patient. You’re an active part of your care.





Let’s be real - this whole ‘generic substitution’ thing is just corporate greed in a white coat. FDA says they’re identical? Cool. Then why do my thyroid levels go haywire every time I refill? They’re not identical. They’re just cheaper. And now states are forced to play along because insurance companies won’t pay for the brand. This isn’t healthcare - it’s a cost-cutting circus.
November 14Rebekah Kryger