When you take multiple medications-especially generic versions-it’s easy to assume they’re harmless because they’re cheap and widely available. But here’s the truth: generic drug interactions can be just as dangerous as brand-name ones. A simple mix of your blood pressure pill and a common painkiller could send you to the ER. And with the rise of online pharmacies, more people are buying meds without talking to a doctor. That’s where digital consultation tools come in-not as a replacement for your pharmacist, but as your second set of eyes.
Why Generic Drugs Aren’t Always Safe Together
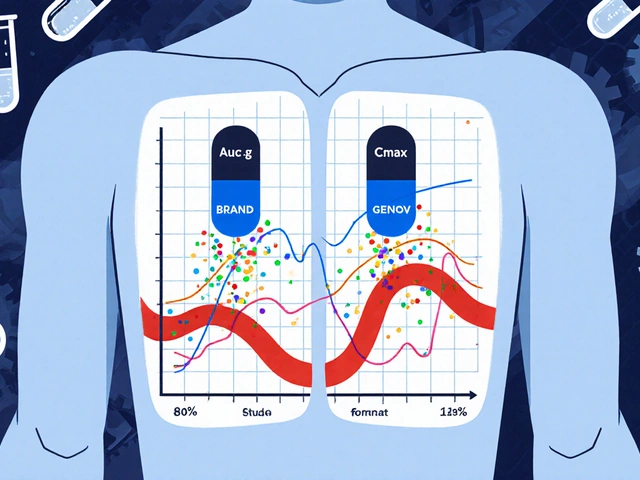
Generic drugs contain the same active ingredients as brand names, but that doesn’t mean they play nice with each other. A 2022 study in the Journal of the American Medical Association found that the average person over 65 takes 4.8 prescription drugs at once. Add over-the-counter pain relievers, herbal supplements, and vitamins-and you’ve got a chemical cocktail with unpredictable results. For example, mixing generic sertraline (an antidepressant) with generic ibuprofen can increase bleeding risk. Or combining generic metformin with certain heart medications might cause lactic acid buildup. These aren’t rare cases. They happen daily. And most people don’t realize it until it’s too late.What Digital Consultation Tools Actually Do
These aren’t fancy AI chatbots. They’re clinical decision support systems built by pharmacists and data scientists to scan drug combinations and flag risks. Tools like Epocrates, Micromedex, and DDInter check your meds against databases of known interactions. They don’t just say “warning.” They tell you why it’s risky-whether it’s a metabolic conflict, a blood pressure spike, or a serotonin overload. Take Epocrates. It lets you check up to 30 drugs at once-brand names, generics, even herbal supplements like St. John’s Wort. That’s huge. If you’re on five different generics, a heart medication, and a sleep aid, you can plug them all in and get a clear risk rating: mild, moderate, or severe. No guesswork. DDInter, developed at Chongqing University, is free and open to anyone. It’s less polished but incredibly detailed. It explains the exact mechanism-like how one drug blocks the liver enzyme that breaks down another, causing dangerous buildup. It’s perfect for people who want to understand, not just be warned.Top Tools Compared: What Works Best for You
| Tool | Max Drugs Checked | Free Access? | Overdose Info? | Best For |
|---|---|---|---|---|
| Epocrates | 30 | Yes (full features) | No | Outpatient use, quick checks |
| Micromedex | Unlimited | Only via hospital | No | Hospitals, complex regimens |
| DrugBank | 5 | Yes (limited) | No | Research, academic use |
| UpToDate Lexidrug | 50+ | Subscription only | Yes | Clinical decision-making |
| DDInter | 5 | Yes (no login) | No | Understanding mechanisms |
Epocrates wins for most people. It’s fast, free, and works on your phone. If you’re managing a chronic condition and take a handful of generics, this is your go-to. Micromedex is the gold standard in hospitals, but you won’t get access unless you work in one. DrugBank is great for deep dives-but if you’re constantly getting pop-ups asking you to pay, it’s frustrating. DDInter is for the curious-students, researchers, or anyone who wants to know the science behind the warning.
They’re Not Perfect-And That’s Dangerous
Here’s the scary part: these tools miss things. A 2022 report from the American Medical Informatics Association found false negative rates between 8% and 32%, depending on the drug. That means one in five dangerous interactions might slip through. And then there’s alert fatigue. A 2023 JAMA Internal Medicine study showed clinicians ignore 49% to 96% of interaction warnings because the systems are too noisy. You get five alerts for every real threat. After a while, you stop paying attention. Even worse, some tools don’t cover herbal supplements or OTC meds well. mobilePDR, for example, is official PDR content-but users report it misses common interactions with turmeric, ginkgo, or even high-dose vitamin D. If you’re taking supplements bought from an online pharmacy, don’t assume your app caught it.How to Use These Tools Right
1. Enter every medication-including vitamins, CBD, and herbal teas. Don’t skip the “harmless” stuff. 2. Check every time you add a new drug. Even if you’ve used the combo before, your body changes. Kidney function drops. Liver enzymes shift. New interactions can appear. 3. Don’t trust the green light. If a tool says “no interaction,” cross-check with another. Use DDInter to understand the mechanism, then verify with Epocrates for real-world risk. 4. Share the results with your pharmacist. Don’t just screenshot it-talk about it. Pharmacists at online pharmacies are trained to spot red flags. Use them. 5. Turn off low-risk alerts if you’re overwhelmed. Most apps let you filter by severity. Only show moderate and severe.
The Bigger Picture: Online Pharmacies and Your Safety Net
Online pharmacies make access easier-but they also make it easier to self-prescribe. You can buy generic metoprolol, fluoxetine, or atorvastatin without a prescription from some sites. That’s legal in some countries, but risky everywhere. Digital tools are your last line of defense. They won’t stop you from ordering the wrong combo, but they can stop you from taking it. Use them like a seatbelt. You don’t need to wear it every second-but when you’re speeding down a highway of medications, you better have it on.What’s Next? AI That Predicts, Not Just Warns
The next wave isn’t just checking what’s in your pillbox-it’s predicting what might happen before you even take it. Merative bought InteracDx in 2023 to make Micromedex smarter. DDInter’s 2024 update uses machine learning to find interactions that haven’t been documented yet. The FDA is pushing for this. Their 2023 Digital Health Plan says better interaction algorithms are a priority. In five years, your app might not just say “warning.” It might say: “This combo increases your risk of kidney injury by 42% based on your age, creatinine level, and other meds.” That’s the future. But for now, the tools we have are enough-if you use them right. Don’t wait for a bad reaction. Don’t assume your pharmacist knows every pill you bought online. Open your app. Type in your meds. Press check. It takes 90 seconds. And it might save your life.Can I trust free drug interaction checkers?
Yes, but with limits. Epocrates and DDInter are free and reliable for most common combinations. DrugBank’s free version only shows basic alerts. If you’re on more than five meds or take supplements, use multiple tools. No single free tool catches everything.
Do digital tools work with generic versions of drugs?
Yes. These tools recognize generic names by their active ingredients. For example, “sertraline” is the same whether it’s Zoloft or a store-brand version. The tool doesn’t care about the label-it cares about the chemical. Always enter the generic name if you’re unsure.
What if my online pharmacy doesn’t ask about my other meds?
That’s a red flag. Reputable online pharmacies require a prescription and a health questionnaire. If they don’t ask about your current medications, avoid them. You’re responsible for your own safety. Never assume a pharmacy will catch a dangerous interaction.
Can these tools detect interactions with supplements?
Some do, some don’t. Epocrates covers over 1,000 supplements. DDInter includes many herbal compounds. But mobilePDR and DrugBank’s free version often miss them. If you take ashwagandha, garlic extract, or CoQ10, double-check with Epocrates or cross-reference with a trusted supplement database like the NIH’s Office of Dietary Supplements.
Are these tools only for doctors?
No. Epocrates and DDInter are designed for patients too. You don’t need a medical license to use them. In fact, patients who check their own meds before picking up prescriptions have fewer ER visits. Use them like a personal safety net.


Okay, but can we talk about how Epocrates saved my life last year? I was on sertraline, metformin, and this sketchy turmeric supplement I bought off Amazon-no prescription, just ‘natural energy boost’-and the app flagged a bleeding risk I had NO idea about. I called my pharmacist immediately. She was like, ‘Girl, you’re lucky you checked.’ Now I check EVERYTHING. Even my gummy vitamins. I’m not even kidding. I have a spreadsheet. With colors. And emojis. 🚨💊🌈
January 10lisa Bajram