HCV Cardiovascular Risk Calculator
Personal Risk Assessment
This calculator estimates your relative cardiovascular risk based on hepatitis C status and other factors. Remember that chronic HCV can double your risk of heart attacks and stroke.
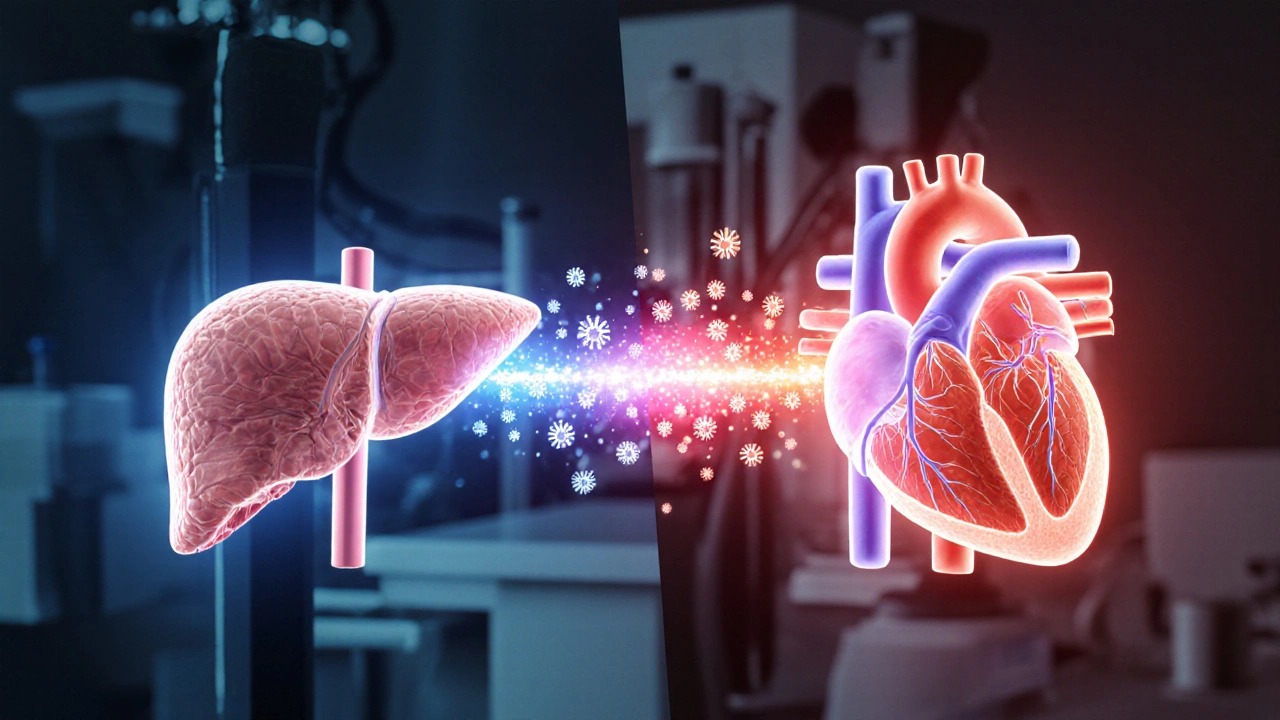
When you hear the word “Hepatitis C,” the liver usually steals the spotlight. Yet a growing body of research shows that the virus doesn’t stay confined to the liver-it can tug on your heart’s strings, too. This article walks you through exactly how chronic Hepatitis C (HCV) can raise your cardiovascular risk, who should worry most, and what you can do right now to keep your ticker in shape.
Key Takeaways
- Chronic HCV infection doubles the odds of developing coronary artery disease and stroke.
- Inflammation, insulin resistance, and altered lipid metabolism are the main pathways linking HCV to heart problems.
- Direct‑acting antiviral (DAA) therapy cuts the virus out of your system and reduces cardiovascular events by about 30%.
- Regular blood‑pressure checks, lipid panels, and an annual cardiac exam become essential once you have chronic HCV.
- Healthy lifestyle habits-no smoking, moderate alcohol, balanced diet, and regular exercise-still matter most for heart protection.
What Is Chronic Hepatitis C?
Chronic Hepatitis C is a liver infection caused by the hepatitis C virus (HCV) that persists for more than six months. The virus spreads mainly through blood-to‑blood contact, such as sharing needles or receiving unscreened blood transfusions. According to the World Health Organization, roughly 71million people worldwide live with chronic HCV, and if left untreated, about 20% develop cirrhosis or liver cancer.
Beyond the liver, HCV drifts into the bloodstream, attaching to immune cells and triggering a low‑grade, systemic inflammation that can affect virtually any organ, including the heart.
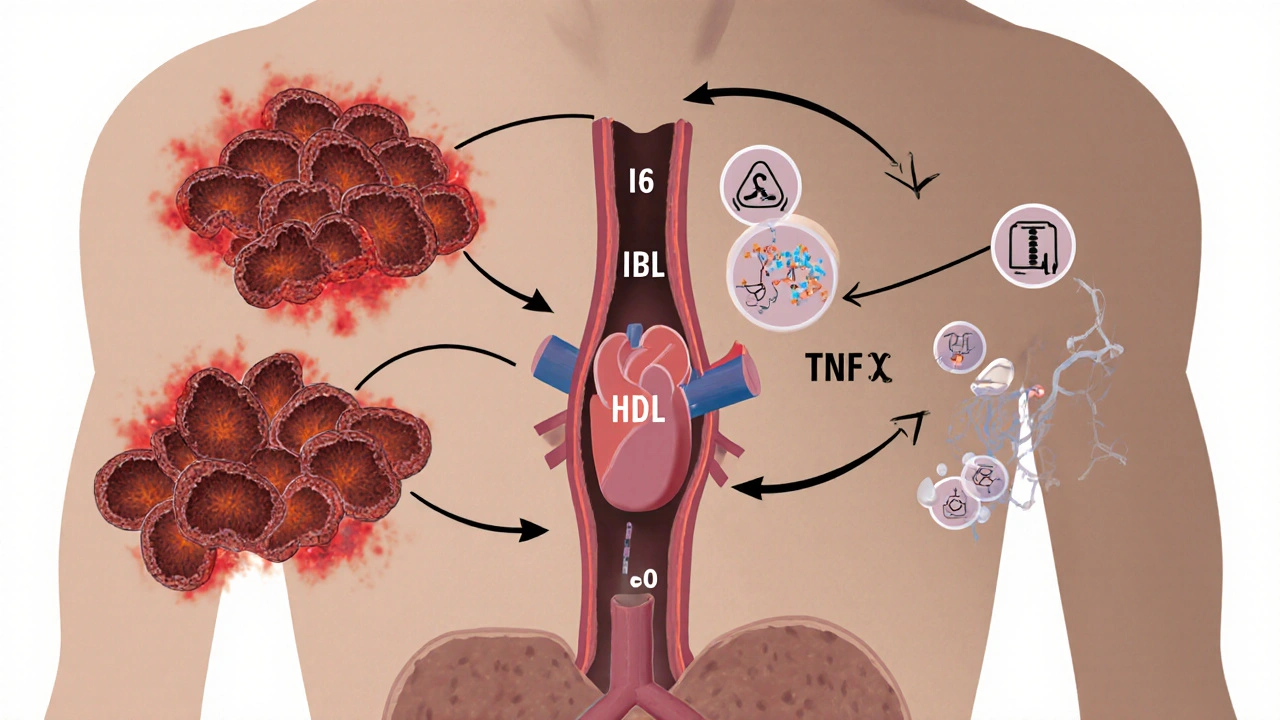
How Does HCV Reach the Heart?
Three biological pathways explain why HCV fans out to the cardiovascular system:
- Chronic inflammation: HCV constantly stimulates cytokine production (IL‑6, TNF‑α), which damages the vascular lining and accelerates atherosclerosis.
- Metabolic disruption: The virus interferes with lipid metabolism, often lowering HDL (“good”) cholesterol while raising triglycerides, creating an unfavorable lipid profile.
- Insulin resistance: HCV impairs insulin signaling, paving the way for type‑2 diabetes-a major heart‑disease risk factor.
These mechanisms are not isolated; they feed into each other, creating a perfect storm for plaque buildup and clot formation.
What the Data Says: HCV and Cardiovascular Disease
Large‑scale cohort studies have quantified the link. A 2023 CDC‑backed analysis of 1.3million U.S. adults found that chronic HCV patients had a 2.2‑fold higher incidence of myocardial infarction (heart attack) compared with HCV‑negative peers, even after adjusting for smoking, hypertension, and diabetes.
Another multi‑national study published in The Lancet Gastroenterology (2022) reported a 1.8‑fold increase in stroke risk among HCV‑positive participants. The hazard ratios were especially high for people with co‑existing cirrhosis, suggesting that liver disease severity magnifies heart risk.
Importantly, these associations persist despite the fact that many HCV patients are younger than typical heart‑disease patients, underscoring the virus’s independent contribution.
Who Is Most at Risk?
Not everyone with chronic HCV faces the same heart danger. The following groups should keep a closer eye on their cardiovascular health:
- Patients with advanced liver fibrosis or cirrhosis - liver scarring amplifies systemic inflammation.
- Individuals with diabetes or pre‑diabetes - HCV‑induced insulin resistance adds to existing glucose problems.
- Older adults (50+ years) - Age already raises heart‑disease risk; HCV pushes it further.
- People who smoke or binge drink alcohol - These habits compound the inflammatory load.
If you fall into any of these categories, a proactive cardiac work‑up becomes a must.
Screening and Monitoring Your Heart While Living with HCV
Below is a practical checklist you can share with your hepatologist or primary‑care doctor:
- Baseline lipid panel - Look for low HDL and high triglycerides.
- Blood‑pressure measurement - Aim for < 130/80mmHg.
- Fasting glucose or HbA1c - Detect early insulin resistance.
- Electrocardiogram (ECG) - Spot arrhythmias or silent ischemia.
- Echocardiogram (if you have cirrhosis) - Checks heart muscle function.
- Carotid ultrasound (optional) - Evaluates plaque buildup in the neck arteries.
Repeat these tests at least annually, or more often if you have additional risk factors.
Impact of Antiviral Therapy on Heart Risk
Since 2014, direct‑acting antivirals (DAAs) have transformed HCV care, achieving cure rates above 95%. Beyond clearing the virus, DAAs also tamp down the inflammatory cascade that harms the heart.
Here’s a snapshot of recent evidence:
| Study (Year) | Population | Hazard Ratio for CV Events (Pre‑DAA) | Hazard Ratio Post‑DAA | Follow‑up (years) |
|---|---|---|---|---|
| Vincenzo et al., 2023 | 5,200 HCV‑positive adults | 2.1 | 1.5 | 3.2 |
| Kumar et al., 2022 | 3,800 with cirrhosis | 2.8 | 1.9 | 2.5 |
| Lee et al., 2021 | 2,600 treatment‑naïve | 1.9 | 1.2 | 4.0 |
Across the board, curing HCV chops the relative risk of heart attacks and strokes by roughly 30% to 40%. That doesn’t mean the risk disappears-other factors still play a role-but the virus’s contribution shrinks dramatically.
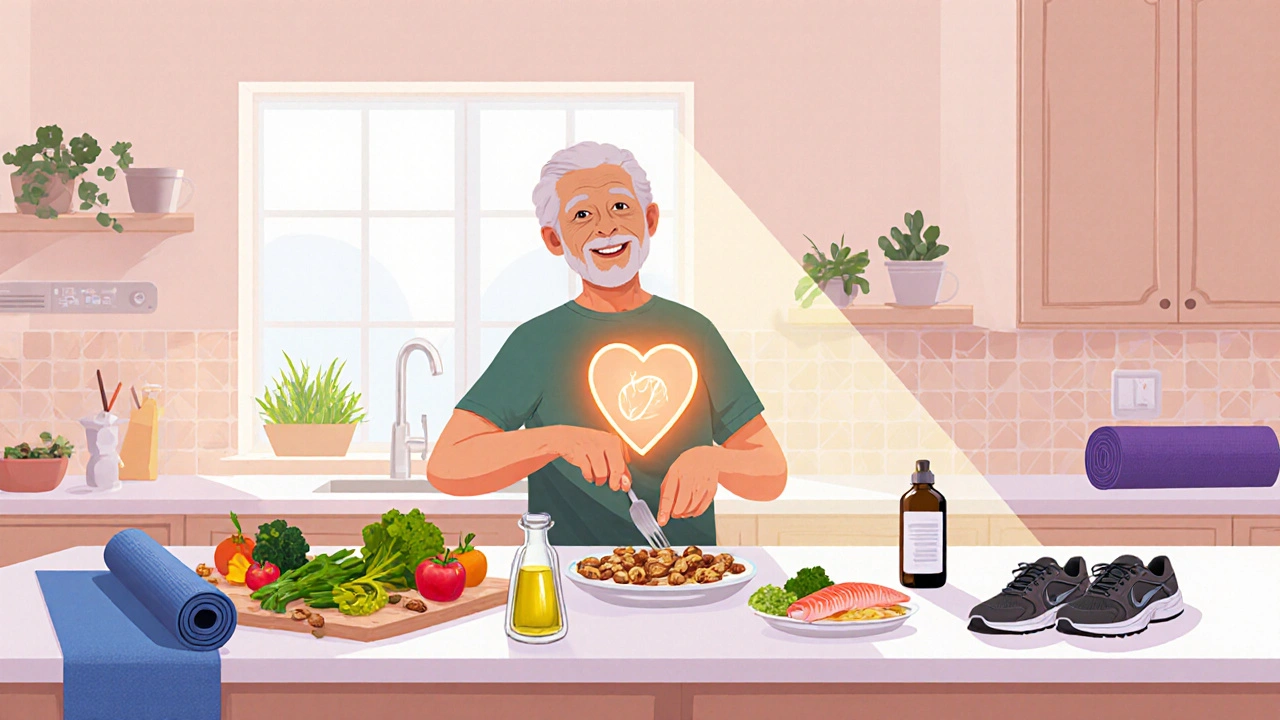
Practical Steps to Protect Your Heart While Managing HCV
Even if you’re waiting for treatment or have already cleared the virus, these heart‑friendly habits can make a big difference:
- Quit smoking - Nicotine adds a double hit to inflammation.
- Limit alcohol - Excess alcohol worsens both liver and heart injury.
- Adopt a Mediterranean‑style diet - Olive oil, nuts, fish, and plenty of veggies raise HDL and lower triglycerides.
- Exercise regularly - Aim for at least 150minutes of moderate aerobic activity per week.
- Manage stress - Chronic stress spikes cortisol, which can aggravate insulin resistance.
- Stay on top of vaccinations - HepatitisB and flu shots reduce extra liver stress, indirectly helping the heart.
Pair these habits with routine check‑ups, and you’ll give your heart the best chance to stay healthy.
Frequently Asked Questions
Can chronic Hepatitis C cause a heart attack?
Yes. Studies show that people with untreated HCV have about twice the risk of a myocardial infarction compared with those who are virus‑free, mainly because of chronic inflammation and metabolic changes.
Does curing HCV eliminate all heart‑disease risk?
Curing HCV removes the virus‑driven inflammatory boost, cutting cardiovascular risk by roughly 30%. However, pre‑existing damage, age, smoking, and other health conditions still matter.
Should I get a cardiac stress test because I have HCV?
A stress test isn’t required for every HCV patient, but it’s wise if you have additional risk factors-such as hypertension, diabetes, or a family history of heart disease. Talk to your doctor about personalized screening.
Do DAAs have any heart‑related side effects?
DAAs are generally safe for the heart. A few trials noted modest increases in blood pressure during the first few weeks, but these resolved without intervention. The overall cardiovascular benefit outweighs any transient effect.
Can lifestyle changes alone reduce HCV‑related heart risk?
Lifestyle tweaks-stop smoking, eat heart‑healthy foods, stay active-can dramatically lower your overall cardiovascular risk, even if the virus remains present. They’re essential whether you’re waiting for treatment or already cured.
Bottom line: chronic Hepatitis C isn’t just a liver problem-it’s a silent partner in heart disease. By understanding the risk, staying on top of screenings, getting cured with DAAs, and embracing heart‑smart habits, you can protect both your liver and your ticker.





For anyone living with chronic HCV, incorporating regular cardiovascular screening into your health routine is essential; a simple lipid panel or annual ECG can catch early changes before they become serious.
October 14Mike Rylance