Carotid Stenosis Risk Calculator
Based on 2023 AHA/ASA guidelines. Enter your carotid artery stenosis percentage to calculate your 90-day stroke risk after a TIA.
Your Risk Assessment
Important: This tool estimates risk based on clinical guidelines. Actual risk depends on individual factors like age, blood pressure, and other health conditions. Consult your healthcare provider for personalized advice.
When you hear a sudden “whoosh” of numbness or weakness that fades in minutes, you’ve likely experienced a Transient Ischemic Attack. It’s a warning flare, not a full‑blown stroke, but it screams that something upstream-often the carotid arteries-needs attention now.
What a TIA Actually Is
Transient Ischemic Attack is a brief episode of neurologic dysfunction caused by temporary loss of blood flow to the brain. Symptoms typically last under 24 hours, most often resolving within an hour. The brain tissue survives, but the event reveals a vulnerable circulation that could tip into a major stroke if left unchecked.
Carotid Artery Disease: The Hidden Culprit
Carotid artery disease refers to the narrowing or blockage of the carotid arteries, the main vessels that feed the brain. When plaque builds up, the artery’s lumen shrinks, reducing blood flow and creating a breeding ground for clots. Those clots can travel to the brain and cause a TIA or an outright stroke.
How the Carotid Artery Works
Carotid artery is a paired vessel that runs on each side of the neck, branching from the aortic arch and delivering oxygen‑rich blood to the frontal lobes. Because it sits close to the surface, it’s an ideal spot for clinicians to assess a patient’s risk using non‑invasive imaging.
The Role of Atherosclerosis and Plaque
Atherosclerosis is the progressive buildup of fatty deposits within arterial walls. In the carotids, this manifests as plaque, which can be soft, calcified, or mixed. Soft plaques are especially dangerous because they rupture easily, releasing emboli that trigger a TIA.
Why a TIA Signals an Imminent Stroke
Studies from the 2023 AHA/ASA guidelines show that 20‑30% of patients who suffer an isolated TIA will have a disabling stroke within 90 days if the underlying carotid problem isn’t treated. The risk spikes when the carotid narrowing exceeds 70% on the side of the symptoms.
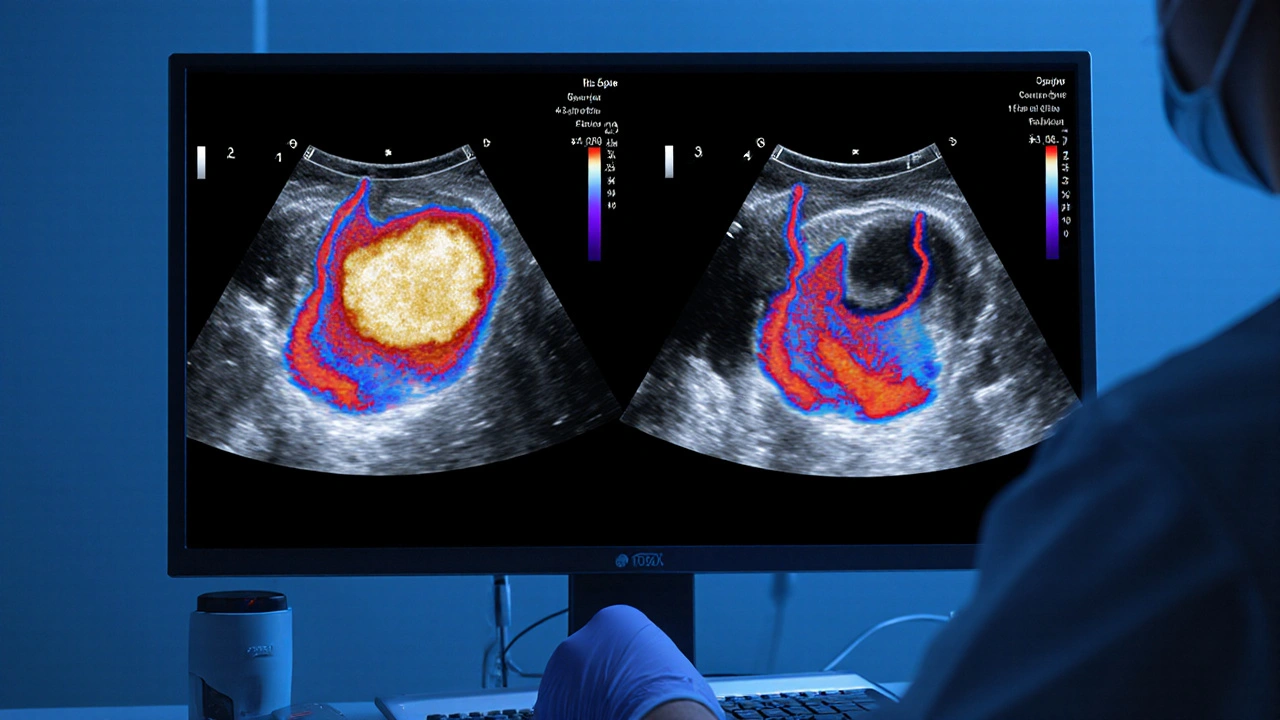
Diagnosing Carotid Artery Disease After a TIA
Timely imaging is the cornerstone of care. The most common modalities include:
| Modality | Sensitivity | Specificity | Pros | Cons |
|---|---|---|---|---|
| Duplex ultrasound | 85‑90% | 95% | Bedside, no radiation, cheap | Operator‑dependent, limited in high bifurcations |
| Magnetic Resonance Angiography (MRA) | 92% | 96% | Excellent soft‑tissue detail, no iodinated contrast | Expensive, contraindicated with some implants |
| CT Angiography (CTA) | 94% | 94% | Fast, high spatial resolution | Ionizing radiation, iodinated contrast risk |
Guidelines recommend that any patient with a TIA get a carotid duplex within 24‑48hours. If the ultrasound suggests ≥50% stenosis, a confirmatory CTA or MRA is usually ordered.
Medical Management While Awaiting Imaging
The first line of defense is antiplatelet therapy-most commonly aspirin 81mg daily, often combined with clopidogrel for the first 21days in high‑risk cases. Blood‑pressure control (target <140/90mmHg) and statin therapy (e.g., rosuvastatin 20mg) are also mandated to stabilize plaque and reduce further clot formation.
When to Consider Surgical Intervention
If imaging reveals ≥70% stenosis on the symptomatic side, or ≥80% on the asymptomatic side with additional risk factors, revascularization becomes the recommended path. Two main options exist:
- Carotid endarterectomy: A surgical peel‑off of plaque through an incision in the neck. It boasts a 30‑day stroke risk of <2% in experienced centers.
- Carotid stenting: A catheter‑based placement of a mesh tube that compresses plaque against the vessel wall. It’s preferred for patients with hostile neck anatomy or severe cardiac disease, but peri‑procedural stroke rates are slightly higher (≈3%).
Decision‑making hinges on patient age, comorbidities, and anatomical considerations. Recent meta‑analyses (2024) show endarterectomy still edges out stenting in patients over 70, while younger patients see comparable outcomes.

Post‑Procedure Care and Long‑Term Surveillance
After either procedure, patients remain on antiplatelet therapy (often dual for 30days, then single) and high‑intensity statins. Duplex ultrasound surveillance is performed at 1month, 6months, then annually to catch restenosis early.
Key Lifestyle Tweaks to Prevent Recurrence
Even with surgery, the underlying atherosclerotic process continues. The most powerful modifiers are:
- Quit smoking-risk drops by 50% within a year.
- Maintain a Mediterranean‑style diet-rich in omega‑3s, fruits, and whole grains.
- Exercise 150minutes of moderate activity weekly.
- Control diabetes-HbA1c <7% correlates with slower plaque progression.
Putting It All Together: A Quick Decision Flow
Below is a practical checklist you can run after a TIA:
- Confirm TIA with neurologic exam; record symptom side.
- Start aspirin (or aspirin+clopidogrel) immediately.
- Order carotid duplex within 48hours.
- If stenosis <50% → intensify medical therapy, lifestyle changes.
- If stenosis 50‑69% → consider CTA/MRA; discuss risk‑benefit of surgery.
- If stenosis ≥70% (symptomatic) → refer for endarterectomy or stenting within 2weeks.
Following this pathway slashes the 90‑day stroke risk from ~20% down to <3%.
Frequently Asked Questions
Can a TIA happen without any carotid narrowing?
Yes. Cardioembolic sources (like atrial fibrillation), small‑vessel disease, or hypercoagulable states can cause TIAs. However, when symptoms match the carotid distribution, carotid disease is the most common culprit.
How accurate is a carotid duplex compared to CTA?
Duplex ultrasound is highly sensitive (85‑90%) and very specific (≈95%) for ≥70% stenosis, but it can miss high bifurcations. CTA offers higher spatial resolution, making it useful when ultrasound results are equivocal.
Is carotid stenting safe for older adults?
In patients over 80, data show a slightly higher peri‑procedural stroke risk compared to endarterectomy. If the neck is hostile or the patient can’t tolerate surgery, stenting remains an acceptable alternative with careful operator experience.
How soon after a TIA should surgery be performed?
Guidelines advise revascularization within 2weeks of the event, ideally within 48‑72hours, to capture the window of highest stroke risk.
Will I need lifelong medication after carotid surgery?
Yes. Lifelong antiplatelet therapy (usually aspirin) and a high‑intensity statin are standard to keep plaque stable and prevent new lesions elsewhere.






Transient ischemic attacks-TIA-are, in essence, a neurological “false alarm,”; they signal that a clot has briefly blocked blood flow to the brain, and, crucially, they often precede a full‑blown stroke, especially when the carotid arteries are compromised,; the carotid artery disease, characterized by plaque buildup, narrows the vessel lumen, and, consequently, any embolus can more easily lodge downstream,; clinicians therefore treat a TIA as a red flag, recommending immediate imaging, antiplatelet therapy, and, when appropriate, carotid endarterectomy or stenting,; ignoring these warnings is, frankly, a dangerous gamble.
October 12Srinivasa Kadiyala