When your asthma is under control, you might not think about breathing. But when it starts to slip, you don’t always feel it coming. That’s where peak flow monitoring comes in. It’s not flashy. It doesn’t involve pills or inhalers. But for many people with asthma, a small handheld device that measures how fast you can blow air out of your lungs can be the difference between a normal day and a trip to the ER.
Why Peak Flow Monitoring Matters
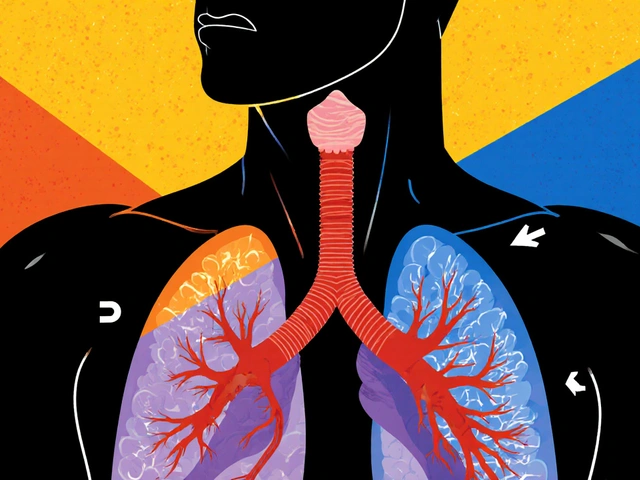
Peak expiratory flow (PEF) is a simple number: how fast you can exhale after taking a full breath. It’s measured in liters per minute using a small plastic device called a peak flow meter. This isn’t about how much air you can hold-it’s about how quickly you can push it out. That speed tells you how open your airways are.Here’s the key point: your lung function can drop before you feel wheezing or tightness. Studies show airflow can decline 24 to 48 hours before symptoms appear. That’s especially true for people who don’t notice early warning signs-like a slight cough, fatigue, or trouble sleeping. For them, peak flow monitoring isn’t optional. It’s a lifeline.
The American Lung Association, GINA guidelines, and the National Institutes of Health all agree: if you have moderate to severe asthma-or if you’ve had a serious flare-up before-daily peak flow tracking should be part of your routine. It’s not a replacement for spirometry in the doctor’s office, but when you’re at home, it’s the best tool you have to catch trouble early.
How to Set Up Your Daily Tracking Routine
You can’t just blow into the meter once and call it good. Accuracy depends on consistency. Here’s how to do it right:- Use the same peak flow meter every single time. Different brands give different readings. Switching meters ruins your data.
- Measure at the same times each day. The best windows are between 7 and 9 a.m. and 6 and 8 p.m. Why? Lung function naturally dips in the early morning and rises later in the day. Tracking at fixed times lets you spot real changes, not daily swings.
- Take three readings each time. Record the highest number. If one reading is way off, you probably didn’t blow hard enough. Don’t guess-do it again.
- Blow with your best effort every time. No half-hearted puffs. You’re not trying to impress anyone. You’re collecting data that could save your life.
- Write it down. Use a paper diary, a notebook, or a phone app. Don’t rely on memory. Patterns only show up when you look back.
People with mild, stable asthma might only need to check twice a week. But if your asthma is moderate, severe, or unpredictable, you need to measure twice daily-every day. The Severe Asthma Toolkit recommends at least eight weeks of daily tracking to build a clear picture of your baseline.
Finding Your Personal Best
Your personal best isn’t a number from a chart or a guess based on your age or height. It’s the highest peak flow number you can consistently hit when your asthma is under control.To find it:
- Track your peak flow twice daily for two to three weeks.
- Only do this when you’re feeling well-no coughing, no wheezing, no rescue inhaler use.
- Record every reading. Don’t skip days.
- After three weeks, look for the highest number you’ve recorded. That’s your personal best.
It might be higher or lower than what a chart says is “normal” for someone your size. That’s fine. Your body is your baseline. A child’s personal best will change as they grow. Adults with changing asthma control should recheck it every six to twelve months.
The Green, Yellow, Red Zone System
Once you know your personal best, you divide your readings into three zones. Think of it like a traffic light.- Green Zone (80-100% of personal best): You’re good. Your airways are open. Keep doing what you’re doing. No changes needed.
- Yellow Zone (50-79% of personal best): Caution. Your airways are narrowing. This is your warning sign. You might not feel sick yet, but your body is telling you something’s off. Follow your asthma action plan. Use your rescue inhaler if instructed. Call your doctor if it doesn’t improve.
- Red Zone (below 50% of personal best): Medical alert. Your airways are dangerously tight. This is an emergency. Take your rescue inhaler immediately. Call your doctor or go to the ER. Don’t wait. Don’t hope it gets better. You’re in serious danger.
The Asthma and Allergy Foundation of America says a drop of 20 to 30% from your personal best can signal the start of an asthma episode. That’s why you don’t wait for symptoms. If your reading drops from 400 to 300 and your personal best is 400, that’s a 25% drop. Even if you feel fine, it’s time to act.
When to Adjust Your Plan
Your asthma action plan should tell you exactly what to do in each zone. But here’s what most people miss:Don’t wait for the red zone to call your doctor. If you’re spending more than two days in the yellow zone-even if you feel okay-you need to talk to your provider. It means your controller medication isn’t working as well as it should. Maybe your dose needs tweaking. Maybe you’re exposed to a trigger you haven’t identified.
Also, if your personal best drops over time-even if you’re still in the green zone-that’s a red flag. It could mean your asthma is getting worse. Don’t ignore it. Bring your diary to your next appointment.
Common Mistakes and How to Avoid Them
Most people who try peak flow monitoring give up because they don’t see results. Here’s why that happens:- Using different meters. One meter says 350. Another says 380. You think you’re getting worse. You’re not. You just switched devices.
- Not blowing hard enough. If your numbers jump around wildly, you’re not giving full effort. Practice with your doctor or nurse. Make sure you’re sealing your lips tightly around the mouthpiece.
- Measuring at random times. If you measure at 7 a.m. one day and 5 p.m. the next, you’ll see false drops. Stick to your schedule.
- Ignoring the diary. If you don’t write it down, you can’t see the pattern. You won’t know if your meds are working or if you’re getting worse.
Also, don’t compare your numbers to someone else’s. Your personal best is yours alone. A teenager might have a personal best of 500. An older adult might have 300. Both are normal for them.
What If You Don’t Have a Peak Flow Meter?
If you’ve never used one, talk to your doctor. Most clinics give them out for free or at low cost. If you’re buying one, ask which model your provider recommends. Avoid cheap, no-name brands. Look for ones that are FDA-cleared and have clear, easy-to-read scales.Some newer meters connect to apps and sync with your phone. That’s helpful if you like digital tracking. But the device itself still needs to be reliable. Don’t trust a free app that estimates your flow rate without a real meter.
Who Benefits Most?
Peak flow monitoring isn’t for everyone. But it’s essential for:- People with moderate to severe asthma
- Those who’ve had recent hospital visits or ER trips
- Patients who don’t notice early symptoms
- Children, because they often can’t describe how they feel
- Anyone on a step-up or step-down treatment plan
If your asthma is mild and you’ve had no flare-ups in years, you might not need daily tracking. But even then, having a meter at home and checking it once a week during allergy season or cold weather can give you peace of mind.
Final Thought: It’s Not About the Number
The number on the meter doesn’t define you. It’s just a tool. But when you use it right, it gives you power. Power to act before you’re gasping. Power to talk to your doctor with facts, not feelings. Power to live without fear.Don’t wait for a crisis to start tracking. Start today. Take three readings. Write them down. Find your personal best. Know your zones. Your lungs will thank you.
How often should I check my peak flow if I have asthma?
If you have moderate, severe, or unstable asthma, check your peak flow twice a day-once in the morning and once in the evening. If your asthma is mild and well-controlled, you may only need to check two to three times a week. Always follow your doctor’s advice, but daily tracking is recommended during any change in symptoms or medication.
What’s the difference between personal best and predicted peak flow?
Predicted peak flow is an average number based on your age, height, sex, and ethnicity. Your personal best is the highest number you’ve actually achieved when your asthma is under control. Your personal best is always more accurate for your own care. You might be higher or lower than the predicted value-and that’s normal.
Can I use a peak flow meter if I have COPD?
Peak flow meters are designed for asthma, not COPD. While some people with COPD use them, they’re less reliable because COPD affects the lungs differently. Spirometry is the standard for COPD monitoring. If you have both asthma and COPD, talk to your doctor about the best way to track your lung function.
Why does my peak flow vary so much from day to day?
Some variation is normal-especially if you measure at different times. But large swings (like dropping 100 points in one day) usually mean your asthma is worsening, you’re not using the meter correctly, or you’ve switched devices. Keep a diary and look for patterns. If your numbers are inconsistent, ask your doctor to watch you use the meter.
Should I use my peak flow meter when I’m having symptoms?
Yes-but not instead of using your rescue inhaler. If you’re wheezing or short of breath, use your inhaler first, then check your peak flow 15-20 minutes later. That tells you if the medicine worked. Don’t wait to see if it gets better. Use your action plan, then check your number to confirm improvement.
How do I know if my peak flow meter is working right?
Bring your meter to your next doctor’s appointment. Have them check your reading against their device. If yours is more than 10% off, it might be faulty or worn out. Replace it if needed. Also, clean it monthly with warm water and mild soap-never use alcohol or harsh cleaners. A dirty meter gives false readings.
Can children use peak flow meters?
Yes, children as young as 5 can use them with supervision. Use a meter designed for kids-it’s smaller and easier to hold. Teach them to blow hard and fast. Their personal best will change as they grow, so recheck it every six to twelve months. Tracking helps parents and doctors spot problems before they turn into emergencies.



Just started using my peak flow meter last week after my doc pushed me on it. Honestly? Game changer. I didn’t realize how much I was breathing shallow until I saw the numbers drop before I even felt it. Now I catch flares before they turn into disasters. Seriously, if you’ve got asthma and aren’t doing this-you’re flying blind.
December 2vinoth kumar