Every time you take an antibiotic when you don’t need it, you’re not just helping yourself-you’re helping bacteria get stronger. That’s the harsh truth behind the rising tide of antibiotic overuse and its dangerous consequences: drug-resistant infections and deadly gut illnesses like Clostridioides difficile (C. difficile). This isn’t science fiction. It’s happening right now, in hospitals, nursing homes, and even in your own neighborhood.
Why Antibiotics Are Losing Their Power
Antibiotics were once miracle drugs. A simple pill could cure a throat infection, a urinary tract infection, or a skin abscess. Today, that’s no longer guaranteed. According to the World Health Organization’s 2025 global report, one in six bacterial infections worldwide are now resistant to standard antibiotics. That means if you get sick, the first drug your doctor reaches for might not work at all. This isn’t random. It’s the direct result of decades of misuse. Antibiotics are prescribed for viral infections like colds and flu-things they can’t touch. They’re given to livestock to make them grow faster, not to treat disease. In many places, people buy antibiotics over the counter without a prescription. And when patients stop taking them early because they feel better, they leave behind the toughest bacteria to multiply and spread. The result? Superbugs. Bacteria like methicillin-resistant Staphylococcus aureus (MRSA) and drug-resistant Escherichia coli are now common in hospitals and communities. In 2019, antimicrobial resistance directly caused 1.27 million deaths globally. Another 4.95 million deaths were linked to resistant infections. That’s more than HIV/AIDS and malaria combined.How C. difficile Turns Antibiotics Into a Threat
One of the most dangerous side effects of antibiotic overuse isn’t resistance-it’s what happens inside your gut. Your intestines are home to trillions of good bacteria that keep you healthy. They help digest food, train your immune system, and block harmful invaders. When you take an antibiotic, especially a broad-spectrum one, it doesn’t just kill the bad bugs. It wipes out the good ones too. That creates a vacuum. And Clostridioides difficile is waiting in the wings. C. difficile is a nasty bacterium that thrives when the normal gut flora is gone. It produces toxins that cause severe diarrhea, fever, and abdominal pain. In serious cases, it leads to colon damage, sepsis, and death. In 2017, the CDC estimated that C. difficile caused nearly half a million infections in the U.S. alone, with 29,000 deaths. While newer data is still being collected, experts agree: the risk is growing. The worst part? C. difficile infections often happen after a hospital stay or after taking antibiotics for something as simple as a sinus infection. People who’ve taken three or more courses of antibiotics in a year are at significantly higher risk. And once you get it, treatment is hard. You might need stronger antibiotics-which can make the problem worse-or even fecal transplants to rebuild your gut bacteria.The Silent Pandemic Is Getting Worse
The COVID-19 pandemic didn’t just strain hospitals-it reversed years of progress in fighting antibiotic resistance. Between 2012 and 2019, the U.S. saw an 18% drop in resistant infections. Hospitals reduced unnecessary antibiotic use. Infection control improved. Then the pandemic hit. Suddenly, doctors were prescribing antibiotics to patients with viral pneumonia, even when there was no proof of bacterial infection. Emergency rooms were overwhelmed. Labs couldn’t keep up with testing. Antibiotics became a default, not a last resort. By 2021, resistant infections in hospitals had jumped by 20% compared to pre-pandemic levels. And it’s not just the U.S. The WHO reports that resistance rates are highest in South Asia and the Eastern Mediterranean, where one in three infections can’t be treated with first-line drugs. In Africa, it’s one in five. But even in high-income countries, last-resort antibiotics like carbapenems are losing effectiveness. By 2035, resistance to these critical drugs could double compared to 2005 levels.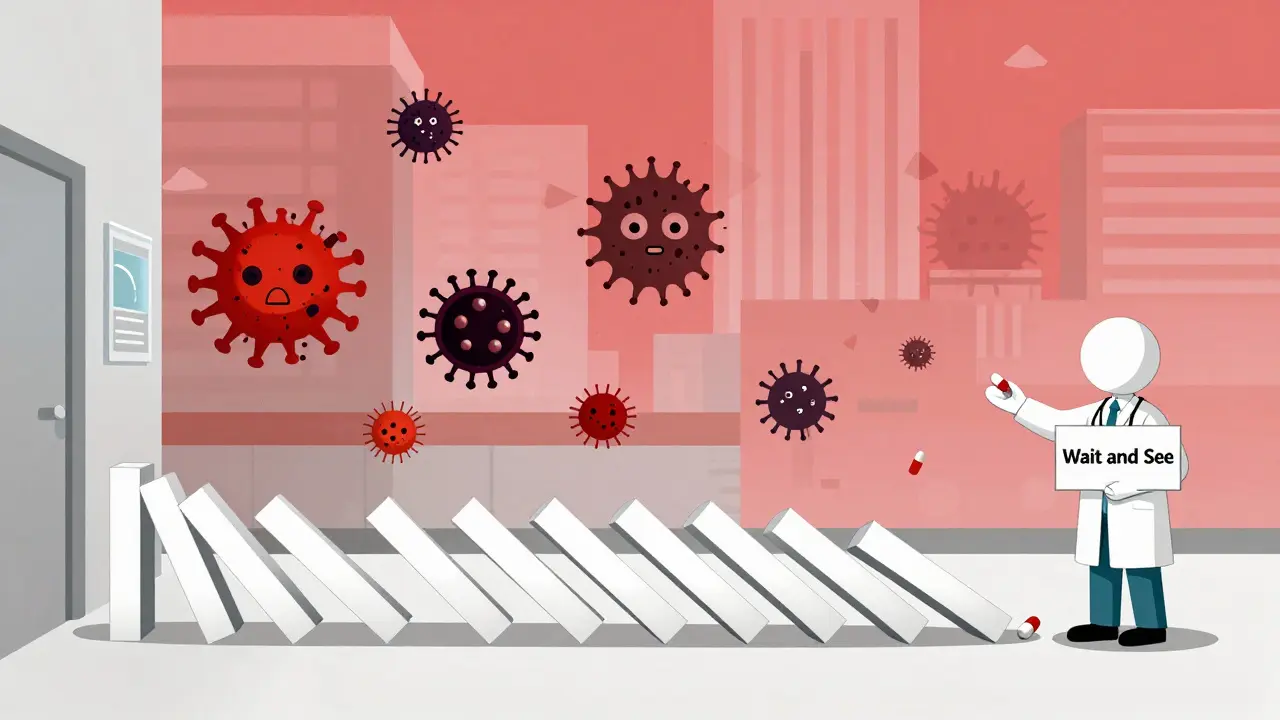
What Happens When Antibiotics Don’t Work Anymore?
Think about surgeries. Cancer treatments. Hip replacements. All of them rely on antibiotics to prevent deadly infections. If those drugs stop working, so do these procedures. Doctors are already seeing cases where patients with urinary tract infections don’t respond to any oral antibiotics. They end up in the hospital, hooked up to IV drugs with harsh side effects-kidney damage, nerve problems, allergic reactions. And sometimes, there’s nothing left. No drug works. That’s not theoretical. It’s happening in clinics across the country. Dr. Kelly Dooley from Vanderbilt University says we’re approaching a point where common infections could become untreatable. “Sometimes we don’t have anything effective to offer,” she says. “That’s a terrible position for a patient and clinician to be in.” The economic cost is staggering. By 2030, resistant infections could cost the global economy $3 trillion a year. By 2050, they could kill 10 million people annually-more than cancer. And that’s if we do nothing.What You Can Do-And What You Shouldn’t
You don’t need to be a doctor to help stop this crisis. Here’s what actually works:- Don’t ask for antibiotics for a cold or the flu. These are viruses. Antibiotics do nothing. Instead, rest, hydrate, and use over-the-counter symptom relief.
- Take antibiotics exactly as prescribed. Even if you feel better after two days, finish the full course. Stopping early leaves behind the strongest bacteria.
- Never share antibiotics. A drug that worked for your friend might be wrong-or dangerous-for you.
- Ask your doctor: “Is this really a bacterial infection?” If they say yes, ask: “What’s the narrowest-spectrum antibiotic that will work?”
- Wash your hands. Simple hygiene reduces the spread of resistant bacteria in homes and hospitals.

Why the System Is Failing
The problem isn’t just patient behavior. It’s broken systems. Pharmaceutical companies aren’t investing in new antibiotics because they don’t make enough money. Unlike drugs for diabetes or high blood pressure, antibiotics are used for short periods. And when new ones come out, doctors are told to hold them in reserve-so they sit on shelves instead of generating revenue. Public health programs that track resistance are underfunded. In many countries, there’s no way to test whether an infection is bacterial or viral before prescribing. So doctors guess. And guess wrong. The WHO has a global action plan, adopted by 194 countries. But implementation is patchy. Only 64% of countries report accurate data on antibiotic use. And in low-income regions, people often lack access to any antibiotics at all-while in wealthy ones, they’re handed out like candy.There’s Still Hope
Change is possible. In the Netherlands and Scandinavia, strict rules on antibiotic use in both humans and animals have kept resistance rates among the lowest in the world. Hospitals there use rapid diagnostic tests to identify infections within hours-not days. That means antibiotics are only given when truly needed. In the U.S., some hospitals have cut unnecessary antibiotic use by 40% through stewardship programs that train staff, monitor prescriptions, and educate patients. These programs cost money-but they save far more in avoided infections, longer hospital stays, and failed treatments. New tools are emerging too. Phage therapy-using viruses that target specific bacteria-is being tested in clinical trials. Rapid tests that detect resistance genes in hours instead of days are becoming more affordable. But none of this will matter unless people understand the stakes. Antibiotic resistance isn’t a future problem. It’s here. And every unnecessary pill you take, every time you pressure a doctor for a script, every time you stop your antibiotics early-you’re helping it spread. The choice isn’t between taking an antibiotic or not. It’s between using them wisely-or losing them forever.Can I get C. difficile from taking antibiotics for a sore throat?
Yes. Even a short course of antibiotics for a viral throat infection can disrupt your gut bacteria enough to let C. difficile grow. It’s not about how serious the infection is-it’s about whether the antibiotic was necessary. Broad-spectrum antibiotics like clindamycin, fluoroquinolones, and cephalosporins carry the highest risk.
Are natural remedies like garlic or honey effective against bacterial infections?
Some natural substances, like honey, have shown mild antibacterial effects in lab studies. But they’re not replacements for antibiotics in serious infections. Relying on them instead of proven treatment can delay care and allow infections to spread. Don’t use them as substitutes-use them as supports, only after consulting your doctor.
If I’ve had C. difficile before, am I more likely to get it again?
Yes. About 20% of people who recover from C. difficile will have a recurrence, and the risk increases with each episode. After two recurrences, the chance of a third jumps to over 60%. Avoiding unnecessary antibiotics is the best way to prevent this cycle.
Do probiotics help prevent C. difficile when taking antibiotics?
Some strains, like Saccharomyces boulardii and Lactobacillus rhamnosus GG, have shown modest benefit in reducing C. difficile risk in clinical trials. But they’re not a guarantee. The best protection is avoiding antibiotics unless absolutely necessary. If you do need them, talk to your doctor about whether a probiotic might help-but don’t rely on it as your main defense.
Why don’t we have more new antibiotics?
Developing a new antibiotic costs over $1 billion, but it rarely makes back that money. Unlike drugs for chronic conditions, antibiotics are used briefly and sparingly to preserve their effectiveness. As a result, big pharmaceutical companies have largely walked away. Only small biotech firms and public partnerships like CARB-X are still investing-and they’re not keeping up with the need.