Medication Timing Calculator for Night Shift Workers
Check Your Medication Safety
Enter your work and sleep schedule to see if your medication may still be active during critical times.
Enter your information to see if your medication timing is safe.
Why Night Shift Workers Turn to Sedating Medications
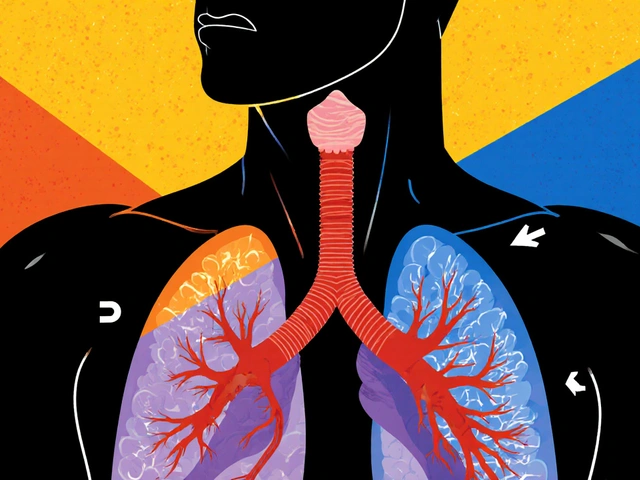
Working nights doesn’t just mean flipping your schedule-it rewires your body’s natural clock. Your brain expects to sleep at night and be awake during the day. When you reverse that, you’re fighting biology. This mismatch is called Shift Work Disorder (a circadian rhythm sleep-wake disorder caused by misalignment between work hours and the body’s internal clock). According to the CDC, over 10 million Americans work nights, and up to 84% of them struggle with sleep problems. Many turn to sleep medications just to get a few hours of rest during the day.
But here’s the catch: sleeping during daylight isn’t the same as sleeping at night. Your body still thinks it’s daytime. Light, noise, and family obligations make deep, restful sleep hard to come by. That’s why many night shift workers end up tired, groggy, and dangerously alert during work. Fatigue isn’t just annoying-it’s deadly. The National Safety Council found fatigued workers are 70% more likely to have a workplace accident. For truck drivers, nurses, and emergency responders, that’s not a risk you can ignore.
The Medications People Use-And What They Really Do
There are two main types of drugs used: ones to help you sleep during the day, and ones to keep you awake at night.
Modafinil (a wakefulness-promoting drug approved by the FDA for shift work disorder) and its longer-acting cousin, armodafinil (a purified version of modafinil with a 15-hour half-life), are the most prescribed wake-up pills. They don’t act like caffeine. They target brain chemicals that control alertness. Studies show modafinil improves reaction time and focus by about 34% compared to a placebo. But it doesn’t make you as sharp as you’d be during the day. It just helps you stay functional.
For sleep, people often use zolpidem (sold as Ambien, Edluar, or Zolpimist), eszopiclone (Lunesta), or zaleplon (Sonata). These are sedative-hypnotics. They help you fall asleep faster-but they don’t improve sleep quality. You might sleep 7 hours, but your brain still cycles through shallow sleep. The FDA added a Boxed Warning in 2023 because these drugs can cause people to drive, eat, or even walk while asleep-without remembering it. One nurse took zolpidem, drove 15 miles in her sleep, and crashed into a fence. She didn’t wake up until she hit the barrier.
Then there’s melatonin (a hormone supplement used off-label to reset the body clock). It’s available over the counter and has fewer side effects. But don’t expect miracles. Studies show it helps you sleep about 40 minutes longer on average. It works best when taken 3 to 4 hours before your desired sleep time. That means if you want to sleep at 8 a.m., you take it at 4 or 5 a.m. Many people skip this timing and wonder why it doesn’t work.
What No One Tells You About Sleep Pills
Doctors often prescribe sleep meds for a few nights. But many night shift workers end up using them for months-or years. The problem? Your body gets used to them. Benzodiazepines like lorazepam or alprazolam, sometimes used off-label, can lead to dependence in 25-30% of users after just 4-6 weeks. That means you can’t sleep without them. One nurse on Reddit said, “I’ve been on Ambien for 9 months and now can’t sleep without it.”
And it’s not just about sleep. These drugs linger in your system. Zolpidem can still affect you 8 hours after you take it. If you’re scheduled to work at midnight, but took a sleep pill at 8 a.m., you might still be groggy during your shift. A 2023 American Medical Association survey found 32% of night shift healthcare workers reported residual drowsiness affecting their performance. That’s not just risky-it’s illegal in some jobs. The National Highway Traffic Safety Administration found drivers using prescription sleep aids were 4.5 times more likely to crash within 2 hours of taking them. The risk doesn’t disappear after 2 hours-it sticks around.
Worse, combining these drugs with alcohol or other sedatives is a recipe for disaster. The FDA warns this can cause breathing problems, extreme drowsiness, or even death. Yet a 2023 National Health Interview Survey found 15% of night shift workers still mix sleep meds with alcohol.

Wakefulness Drugs: The Double-Edged Sword
Modafinil and armodafinil sound like the perfect fix. No jitteriness. No crash. Just steady alertness. And for many truck drivers and ER staff, they are. The National Transportation Safety Board reported a 28% drop in fatigue-related crashes among truckers using modafinil under medical supervision.
But here’s what you won’t hear from ads: these drugs don’t fix your circadian rhythm. They just mask the symptoms. Your body still thinks it’s daytime. Your cortisol levels are off. Your melatonin production is suppressed. You’re not truly rested. And after 3-4 weeks of daily use, many users report diminishing effects. The drug stops working as well. That’s when people start increasing the dose-risking side effects like headaches, anxiety, or heart palpitations.
Also, modafinil has a 12-15 hour half-life. That means if you take it at 6 p.m. for a midnight shift, you could still feel its effects at 6 a.m. the next day-right when you’re trying to sleep. Many people don’t realize this until they’re wide awake at 7 a.m. and can’t fall asleep for hours.
What Works Better Than Pills
The truth? Medications are a band-aid. The real solution is managing light, timing, and sleep hygiene.
Light exposure is the most powerful tool you have. If you’re trying to sleep during the day, block sunlight with blackout curtains. Wear blue-light-blocking glasses on your commute home. If you’re at work at night, get bright light exposure-especially in the first half of your shift. This tells your brain it’s daytime. Many hospitals now give night workers light therapy lamps. A 2023 SHRM report found 73% of large employers now offer them.
Consistency matters more than you think. Try to sleep and wake at the same time every day-even on days off. Your body craves routine. If you sleep from 8 a.m. to 4 p.m. on workdays but sleep from midnight to 8 a.m. on weekends, you’re resetting your clock every other day. That’s exhausting.
Also, avoid caffeine in the last 4 hours before your sleep time. Don’t eat heavy meals right before bed. And don’t use your bed for anything but sleep. No scrolling, no TV. Your brain needs to associate your bed with rest.

How to Use Medications Safely (If You Must)
If your doctor prescribes something, follow these rules:
- Timing is everything. Take wakefulness drugs like modafinil one hour before your shift. Take sleep meds like zolpidem or eszopiclone only when you can sleep for 7-8 hours straight.
- Never combine with alcohol. The FDA warns this can cause fatal breathing problems.
- Don’t drive after taking sleep meds. Even if you feel fine, your reaction time is still impaired.
- Use melatonin correctly. Take 0.5mg to 5mg, 3-4 hours before you plan to sleep. Don’t take it right before bed.
- Set a limit. Most doctors won’t prescribe sleep meds for more than 3-4 weeks. If you still can’t sleep, talk to a sleep specialist-not your primary care doctor.
Also, ask your doctor: “Is this medication safe for my job?” If you drive, operate machinery, or care for patients, some meds are simply too risky.
The Bigger Picture: Why This Problem Is Growing
The global market for shift work disorder treatments is expected to hit $2 billion by 2030. More people are working nights. Hospitals are understaffed. Delivery drivers work around the clock. Employers are starting to notice. Sixty-eight percent of hospitals with 24/7 operations now have formal fatigue management programs. That’s up from 42% in 2020.
But most programs still focus on pills. The real progress is in education. The FDA now requires all sleep medication packages to include clear instructions on sleep duration. The National Institute for Occupational Safety and Health is developing new guidelines for doctors to better assess risk before prescribing.
And the future? It’s personal. Researchers at Northwestern University are studying how your genetics affect your body clock. In five years, you might get a genetic test that tells you whether you’re a morning person or night owl-and what dose and timing of melatonin or modafinil will work best for you.
Until then, the safest choice isn’t a pill. It’s a routine. A dark room. A consistent schedule. And knowing when to say no to medication.
When to Seek Help
If you’ve tried adjusting your sleep habits and still can’t rest during the day, it’s time to see a sleep specialist. Not your regular doctor. Not your pharmacist. A specialist in circadian disorders. They can run tests to see if you have Shift Work Disorder or something else-like sleep apnea. Many night workers have undiagnosed sleep apnea, which makes sleep meds even more dangerous.
Also, if you’re relying on pills to get through your shift, if you’re afraid to go without them, or if you’ve had a close call while driving or working-don’t wait. Talk to someone. Your safety-and the safety of others-depends on it.





I've been a night shift nurse for 12 years. Modafinil saved my life. Not because I'm lazy, but because my body refuses to adapt. I take 100mg at 10:30pm. I'm alert until 7am. No crash. No jitter. Just steady. I don't sleep until noon. Blackout curtains, earplugs, no screens. It's not magic. It's management.
December 25Michael Dillon