Vitamin K Intake Calculator
This tool helps you track your daily vitamin K intake. For most people on warfarin, maintaining consistent vitamin K intake between 60-180 mcg per day is ideal. The goal is to keep your intake within a 25 mcg window of your usual amount.
- Select foods from the list and enter your serving size
- The calculator will show your total vitamin K intake
- Check if your intake is within the target range for stable INR levels
Current Vitamin K Total
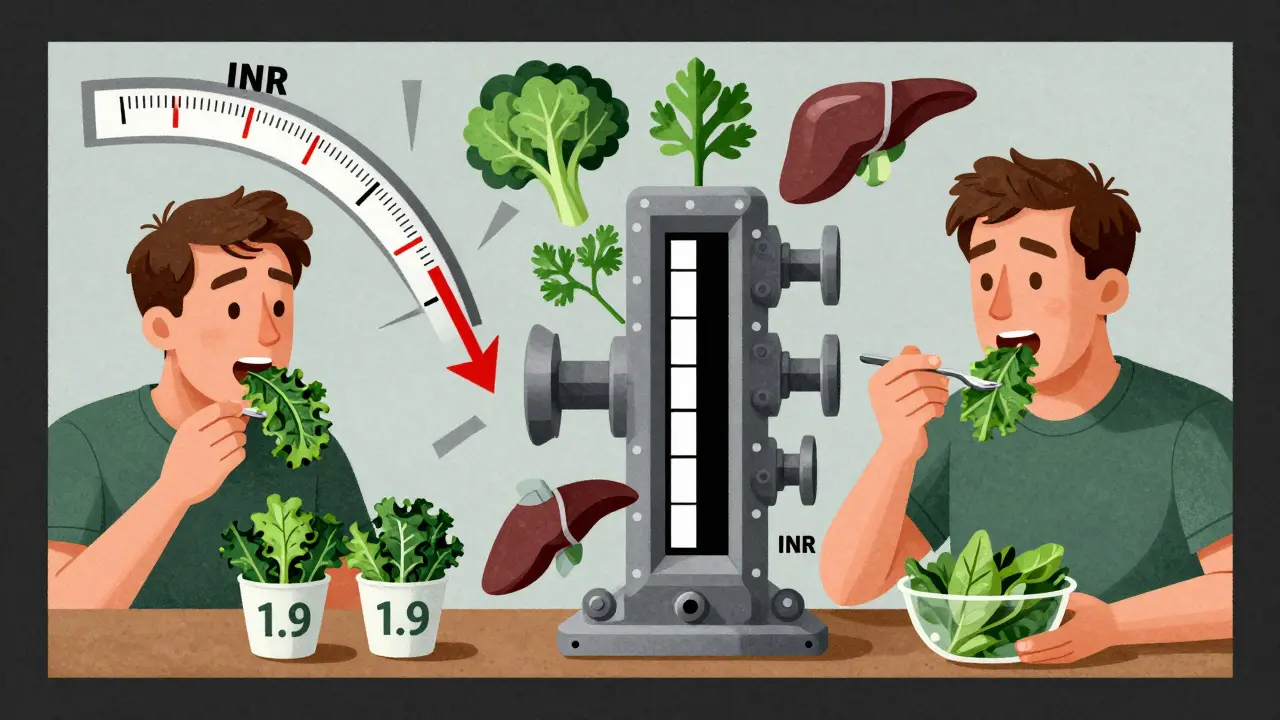
0 mcgWhen you're on warfarin, eating a salad isn't just about getting healthy-it can change how well your blood thinner works. A single cup of cooked kale can pack over 500 micrograms of vitamin K. That’s more than five times the daily amount most people need. For someone taking warfarin, that kind of spike can drop your INR fast, raising your risk of clots. But stop eating all greens? That’s just as dangerous. The truth isn’t about avoiding vitamin K. It’s about keeping it steady.
How Warfarin and Vitamin K Work Together
Warfarin doesn’t thin your blood. It stops your body from using vitamin K to make clotting proteins. Without enough vitamin K, your blood takes longer to clot-that’s the goal. But if you suddenly eat a lot of vitamin K-like a big bowl of spinach or a handful of parsley-your body gets more of the raw material it needs to make those clotting factors. Your INR drops. Too low, and you’re at risk for stroke or pulmonary embolism.
On the flip side, if you go days without any vitamin K-rich foods, your body runs low on the cofactor warfarin is trying to block. Your INR spikes. Too high, and you risk bleeding-nosebleeds, bruising, even internal bleeding. This isn’t theoretical. Studies show people who swing their vitamin K intake by more than 35% from day to day are nearly three times more likely to have dangerous INR fluctuations.
The Complete List of Vitamin K-Rich Vegetables
Not all greens are equal. Some are mild. Others are powerhouses. Here’s the real list, based on USDA FoodData Central (2023), measured per typical serving:
- Kale, cooked (½ cup): 547 mcg
- Spinach, cooked (½ cup): 444 mcg
- Collard greens, cooked (½ cup): 418 mcg
- Swiss chard, cooked (½ cup): 299 mcg
- Turnip greens, cooked (½ cup): 265 mcg
- Parsley, fresh (¼ cup): 246 mcg
- Mustard greens, cooked (½ cup): 210 mcg
- Brussels sprouts, cooked (½ cup): 109 mcg
- Broccoli, cooked (½ cup): 102 mcg
- Green cabbage, cooked (½ cup): 82 mcg
- Asparagus, cooked (½ cup): 70 mcg
- Romaine lettuce, shredded (1 cup): 48 mcg
These aren’t just ‘healthy veggies.’ They’re potent. One serving of kale can push your daily vitamin K intake past 500 mcg. That’s enough to knock your INR down by 0.3 to 0.5 units in under 48 hours.
Other Surprising Sources of Vitamin K
It’s not just leafy greens. Many everyday foods contain vitamin K, often in amounts you wouldn’t guess:
- Beef liver (3 oz): 106 mcg
- Egg yolks (1 large): 25 mcg
- Seaweed, dried (10g): 45-100 mcg
- Boost Original drink (8 oz): 25 mcg
- Ensure Original (8 oz): 25 mcg
- Viactiv Calcium Chews (1 tablet): 25 mcg
These aren’t just snacks. They’re daily variables. If you start drinking a Boost shake every morning after years of not touching it, your INR could drop without warning. Same if you begin taking calcium chews for bone health-many contain added vitamin K. Always check labels. And if you’re on warfarin, never start a new supplement without talking to your anticoagulation clinic.
What You Can Eat Without Worry
You don’t need to become a food detective 24/7. Many foods are safe and won’t interfere:
- Carrots
- Cucumbers
- Tomatoes
- Onions
- Potatoes
- Apples, bananas, oranges
- White rice, pasta, bread
- Chicken, fish, pork (without liver)
These are your go-to foods. They’re low in vitamin K and won’t mess with your INR. You can eat them freely. The trick isn’t to avoid vitamin K-it’s to keep your intake stable. If you normally eat spinach twice a week, keep doing that. If you never eat kale, don’t start.
The Big Mistake: Going Cold Turkey
Many patients hear ‘vitamin K affects warfarin’ and assume they need to cut it out completely. That’s the most common error-and it’s dangerous.
A 2022 survey of over 1,800 warfarin users found that 68% initially avoided all green vegetables. Forty-two percent ended up in the ER or hospital because their INR spiked after going too long without vitamin K. One Reddit user, u/ClotFreeSince2019, logged his INR dropping from 2.8 to 1.9 after eating three cups of kale in five days. Another patient, Mary T., age 67, has kept her INR stable at 2.5 for five years by eating exactly one cup of spinach salad every Tuesday and Thursday. No more. No less.
It’s not about restriction. It’s about rhythm.
What to Avoid: Juice, Alcohol, and Supplements
Some things aren’t just risky-they’re outright dangerous with warfarin.
- Cranberry juice: Can raise your INR by 0.8 to 1.2 units in 72 hours. One glass is enough to cause bleeding.
- Grapefruit juice: Blocks the liver enzyme that breaks down warfarin. This can increase warfarin levels by 15-30%, making you over-anticoagulated.
- Alcohol: More than one drink a day increases bleeding risk. But if you’ve always had one glass of wine with dinner, keep doing it. Consistency matters more than total avoidance.
- Herbal supplements: Garlic, ginkgo, ginseng, and green tea extract can all increase bleeding risk. Even ‘natural’ doesn’t mean safe.
These aren’t ‘maybe’ risks. They’re red flags. If you’re unsure, skip it. Talk to your doctor before trying anything new.
How to Get It Right: The Consistency Protocol
Here’s how the best-managed patients do it:
- Find your baseline. For two weeks, eat your normal diet. Log everything you eat using a food diary or app like the National Blood Clot Alliance’s Warfarin Food Guide.
- Calculate your average daily vitamin K. Use the USDA database or a dietitian’s tool. Most people on warfarin need 60-180 mcg per day, but your target depends on your dose and genetics.
- Stick to the same amount every day. If your baseline is 100 mcg, aim for 80-120 mcg daily. That’s a ±25 mcg window. Use measuring cups. Cook the same way. Same portion. Same days.
- Time it right. Eat vitamin K-rich foods at the same time each day-preferably in the evening. This avoids interference with morning INR tests.
- Track changes. If you go on vacation, get sick, or start eating differently, tell your clinic. Don’t wait for your next appointment.
The University of North Carolina’s Anticoagulation Management Service cut emergency visits by 43% using this exact method. Patients who logged meals with photos had better control than those who just remembered.

When You Should Talk to Your Doctor
You don’t need to panic over every bite. But call your anticoagulation clinic if:
- Your INR changes by more than 0.5 units without a dose change
- You start or stop a supplement, even if it’s ‘natural’
- You’re sick for more than two days and eating less
- You’re traveling and your diet will change
- You’re planning surgery or a dental procedure
These aren’t emergencies-but they’re signals. Your dose may need adjusting. Don’t guess. Call.
What About New Blood Thinners?
DOACs like apixaban (Eliquis) and rivaroxaban (Xarelto) don’t interact with vitamin K. That’s why they’re now the first choice for most patients. But warfarin is still the only option for some:
- People with mechanical heart valves
- Those with antiphospholipid syndrome
- Patients with severe kidney disease (eGFR under 30)
Over 4.7 million people in the U.S. are still on warfarin. For them, managing vitamin K isn’t optional. It’s life-saving.
Final Thought: It’s a Habit, Not a Diet
Managing warfarin with food isn’t about perfection. It’s about predictability. You don’t need to be a nutritionist. You just need to be consistent. Eat your spinach on Tuesday and Thursday. Don’t eat kale unless you normally do. Avoid cranberry juice. Don’t start supplements without asking. Track your meals. Tell your clinic about changes.
This isn’t hard. It’s just different. And for people who do it right, their INR stays stable. Their risk of stroke drops. They live longer. And they get to eat their vegetables-without fear.
Can I eat spinach if I’m on warfarin?
Yes, but only if you eat it consistently. Eating spinach every Tuesday and Thursday is fine. Eating it three times one week and not at all the next week is dangerous. The key is keeping your daily vitamin K intake within ±25 mcg of your usual amount.
Does cooking affect vitamin K in vegetables?
Yes, but not dramatically. Boiling leafy greens can reduce vitamin K by 15-20% because some leaches into the water. Steaming, sautéing, or microwaving preserves more. But the biggest factor is the amount you eat, not the cooking method. Stick to standard serving sizes: ½ cup cooked or 1 cup raw.
Is it safe to take vitamin K supplements while on warfarin?
Only under medical supervision. Some studies show that taking exactly 100 mcg of vitamin K daily can reduce INR swings by 37%. But this isn’t a DIY fix. It requires close INR monitoring and a doctor’s approval. Never start a supplement without talking to your anticoagulation clinic.
Why is cranberry juice dangerous with warfarin?
Cranberry juice can increase the effect of warfarin by interfering with how your body breaks it down. Studies show it can raise your INR by 0.8 to 1.2 units in just 72 hours. That’s enough to cause serious bleeding. Avoid it completely, even in small amounts.
How long does it take to get used to managing vitamin K with warfarin?
Most people need 3 to 6 months to build consistent habits. During that time, you’ll likely have several INR checks and dietitian visits. After six months, patients who track their meals regularly see a 12% improvement in time spent in the safe INR range. It gets easier with practice.
Should I use a food tracking app?
Yes. Apps like the National Blood Clot Alliance’s Warfarin Food Guide let you log meals, scan barcodes, and see vitamin K content instantly. Over 42,000 people use it. Patients who use tracking tools have fewer INR fluctuations and fewer ER visits. It’s the simplest way to stay in control.
Can I drink alcohol while on warfarin?
One drink per day is generally safe if you’ve always had it. But never increase your intake suddenly. Alcohol can thin your blood further and increase bleeding risk. If you don’t drink, don’t start. If you do, keep it consistent.
What if I’m sick and can’t eat vegetables?
If you go more than two days without your usual vitamin K intake, call your clinic. Not eating greens can cause your INR to rise dangerously. Your doctor may temporarily adjust your warfarin dose. Don’t wait for your next test.





Let’s be real - this post reads like a pharmaceutical brochure written by a guy who thinks ‘consistency’ is a personality trait. Vitamin K? INR? You’re telling me I can’t even enjoy a goddamn kale smoothie without doing math like I’m preparing for a NASA launch? I’m on warfarin, not running a biochemistry lab. And don’t get me started on ‘tracking meals with photos.’ Next they’ll ask me to timestamp my broccoli.
December 18Also, why is there a 25 mcg window? Why not 50? Why not 5? Who decided this? Some guy in a white coat with a clipboard and a caffeine addiction? This isn’t medicine - it’s performance art.
And don’t even get me started on the ‘Boost shake’ thing. So now I can’t even have a protein drink without a risk assessment? I’m starting to think the real goal here is to make patients feel like failures before they even leave the clinic.
Also - who the hell wrote this? Did they just copy-paste from a Medscape article and add emojis? I’m not impressed.
Dominic Suyo