Acute Kidney Injury (AKI) doesn’t announce itself with a siren. It creeps in quietly-sometimes after a bad bout of food poisoning, a missed dose of blood pressure meds, or even a routine CT scan. One day you feel fine; the next, your legs are swollen, your urine has dropped to a trickle, and your doctor says your kidneys are failing. This isn’t chronic disease. This is sudden. This is urgent. And it’s more common than most people realize.
What Exactly Is Acute Kidney Injury?
AKI means your kidneys suddenly stop working the way they should. It’s not a slow decline like chronic kidney disease. It’s a sharp drop in function-sometimes in just hours. The kidneys filter waste, balance fluids, and regulate electrolytes. When they fail, toxins build up, fluids pool in your lungs, and your blood chemistry goes haywire. The old term, acute renal failure, is outdated. Today, we call it acute kidney injury because even a small dip in function can be dangerous.
The current standard, set by KDIGO in 2012, defines AKI by three things: a rise in serum creatinine by 0.3 mg/dL in 48 hours, a 50% increase from your baseline over 7 days, or urine output below 0.5 mL per kg per hour for six hours. These aren’t arbitrary numbers. They’re based on what actually predicts death, dialysis, or long-term damage.
Why You Might Not Notice It
Here’s the scary part: about 22% of AKI cases show no symptoms at all. People don’t feel sick. They don’t have pain. They just get a routine blood test-and suddenly, their creatinine is up. That’s why hospitals now monitor high-risk patients daily. If you’re over 65, on diuretics, or in the ICU, your creatinine should be checked every 24 to 48 hours.
When symptoms do appear, they’re vague. Fatigue? Check. Nausea? Common. Swollen ankles? Yes. But here’s what’s often missed: confusion in older adults, shortness of breath from fluid in the lungs, or chest pain from inflammation around the heart. These aren’t just signs of aging or a cold-they’re red flags for kidney trouble.
Three Causes, Three Treatments
AKI doesn’t have one cause. It has three main types-and each needs a different fix.
- Prerenal (60-70% of cases): Your kidneys aren’t getting enough blood. This happens with severe dehydration from vomiting or diarrhea, low blood pressure from infection, or heart failure. The kidneys aren’t damaged yet-they’re just starving. Fix the blood flow, and they bounce back. A quick IV fluid bolus of 500-1000 mL of saline can reverse this in 24 hours if caught early.
- Intrarenal (25-35%): The kidneys themselves are hurt. This is where things get serious. Common culprits? Antibiotics like gentamicin, contrast dye from CT scans, or autoimmune diseases like glomerulonephritis. The most frequent damage is acute tubular necrosis (ATN), where kidney cells die from lack of oxygen or toxins. Recovery takes weeks, and sometimes dialysis is needed while the kidneys heal.
- Postrenal (5-10%): Something’s blocking urine flow. In men over 60, that’s often an enlarged prostate. In others, it’s kidney stones or tumors. If urine can’t leave the body, pressure backs up and crushes the kidneys. The fix? A stent or catheter. Remove the blockage, and kidney function often improves within hours.
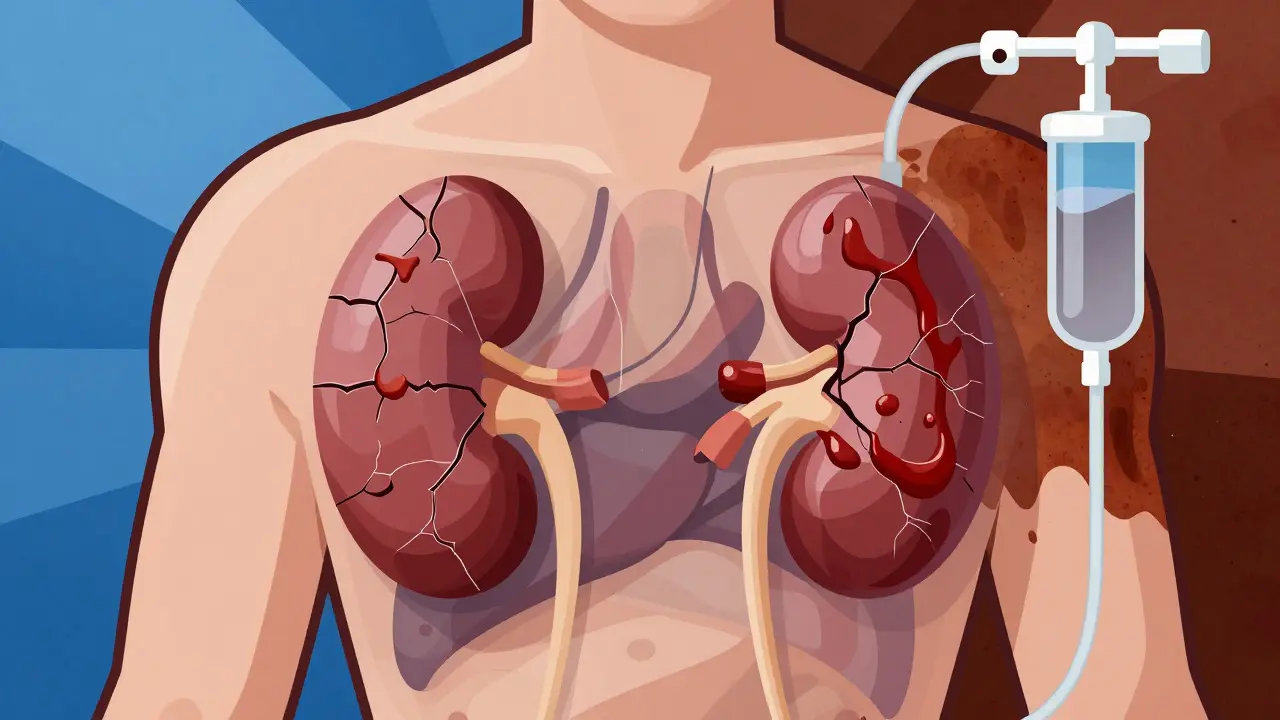
What Happens If It’s Not Treated?
Untreated AKI doesn’t just linger-it explodes into life-threatening problems.
- Hyperkalemia: Potassium builds up in your blood. Levels above 5.5 mEq/L can trigger deadly heart rhythms. Emergency treatment? Calcium gluconate, insulin, and dialysis.
- Fluid overload: Your body can’t pee out the water you drink. Fluid leaks into your lungs-causing coughing, gasping, and oxygen levels that plummet. This happens in 30-40% of severe cases.
- Metabolic acidosis: Your kidneys can’t clear acid. Your blood becomes too acidic, making you breathe fast and feel exhausted. This affects 35% of patients.
- Pericarditis: Inflammation around the heart. Chest pain that gets worse when you lie down. Seen in 15% of untreated cases.
And then there’s the long-term cost. About 23% of people who survive AKI develop chronic kidney disease within a year. Each episode raises your risk of needing dialysis fivefold. Even if your creatinine returns to normal, your kidneys may never fully recover their reserve.
How Is It Diagnosed?
It starts with blood and urine tests. Serum creatinine is the classic marker, but it’s slow to rise. Blood urea nitrogen (BUN) often goes up too. The ratio of BUN to creatinine helps tell if it’s prerenal (high ratio) or intrinsic (normal ratio). Fractional excretion of sodium (FeNa) below 1% suggests prerenal; above 2% points to kidney damage.
Ultrasound is used in 85% of cases. It checks kidney size, texture, and whether there’s a blockage. If a stone is suspected, a CT urogram finds it with 95% accuracy. Newer tools are emerging: NGAL and TIMP-2/IGFBP7 biomarkers can predict AKI 24-48 hours before creatinine climbs. These aren’t routine yet-but in ICUs, they’re changing survival rates.
Recovery: It’s Not Guaranteed
Some people bounce back in days. Others never fully recover. It depends on how bad it was, how fast it was caught, and your health before it happened.
- Prerenal AKI: 70-80% recover fully if treated within 24 hours.
- Intrarenal AKI: Only 40-60% recover completely. If you had prolonged oliguria (less than 400 mL/day for over 14 days), full recovery drops to 20-30%.
- Postrenal AKI: If the blockage is removed quickly, recovery is often near 100%.
But age, pre-existing kidney disease, and needing dialysis change the game. If you’re over 65, your chance of full recovery drops by 35%. If your baseline eGFR was already below 60, your odds halve. And if you needed dialysis? Only 25% regain full kidney function within three months.
What Recovery Really Feels Like
People think once the creatinine normalizes, they’re back to normal. They’re not.
A 2022 survey of over 1,200 AKI survivors found that 68% felt exhausted for months-even after their labs looked fine. They called it “kidney fatigue.” Walking to the mailbox left them breathless. Mental fog lasted. Anxiety about their kidneys haunted them. One man, after 17 days on CRRT in the ICU, said the fear of needing permanent dialysis was worse than the physical pain.
But recovery stories exist. One patient had a creatinine of 1.8 (baseline 0.9) after dehydration. Two liters of IV fluids in the ER. By the next day, it was back to 1.0. No dialysis. No long-term issues. Just a lesson learned: don’t ignore thirst.
What You Can Do Now
Prevention is the best treatment.
- Stay hydrated-especially when sick, hot, or on diuretics.
- Know your baseline creatinine. Ask your doctor for a copy of your last blood test.
- Be cautious with NSAIDs (ibuprofen, naproxen). They’re a top cause of AKI in older adults.
- If you’re scheduled for a CT scan with contrast, tell your doctor if you have kidney disease, diabetes, or are over 60. Pre-hydration can cut risk by half.
- Don’t ignore swelling, fatigue, or low urine output. Especially if you’re on blood pressure meds or have heart disease.
And if you’re hospitalized? Ask: “Am I being monitored for kidney injury?” If you’re in the ICU, your urine output should be measured hourly. If your creatinine hasn’t been checked in 48 hours, push for it.
The Future: Early Alerts and AI
Hospitals are starting to use AI to predict AKI before it happens. Algorithms scan electronic records for patterns-low blood pressure, rising creatinine, new antibiotics-and flag patients 12-24 hours before symptoms show. One study showed this cut AKI incidence by 25%.
Meanwhile, trials like STARRT-AKI are testing whether starting dialysis earlier saves lives. Early results suggest a 9% drop in 90-day death rates when treatment begins before toxins build up too high.
These aren’t distant dreams. They’re happening now-in Manchester, in London, in U.S. hospitals. The goal? Catch AKI before it catches you.
Can acute kidney injury be reversed?
Yes, in many cases-especially if caught early. Prerenal AKI, caused by dehydration or low blood pressure, often fully reverses with fluids. Postrenal AKI from a blockage usually improves immediately after the obstruction is removed. Intrarenal AKI, like from toxins or infection, may take weeks to heal and sometimes leaves lasting damage. Recovery depends on severity, speed of treatment, and your overall health before the injury.
How long does it take to recover from acute kidney injury?
Recovery time varies. Prerenal cases often improve within 24-48 hours. Intrarenal cases, like acute tubular necrosis, may take 2-6 weeks. Severe cases with prolonged low urine output can take months. Some people never fully recover. Follow-up blood tests at 1, 3, and 6 months are critical to track kidney function after discharge.
Can you have acute kidney injury without symptoms?
Yes. About 22% of AKI cases are found only through blood tests-no pain, no swelling, no changes in urine. This is why hospitals monitor high-risk patients closely. Older adults, those on multiple medications, and ICU patients are especially vulnerable to silent AKI.
What drugs can cause acute kidney injury?
Common culprits include NSAIDs like ibuprofen and naproxen, certain antibiotics (aminoglycosides like gentamicin), contrast dye used in CT scans, and some blood pressure medications like ACE inhibitors or ARBs-especially if you’re dehydrated. Always tell your doctor about all medications you’re taking before any procedure or hospital admission.
Does drinking more water help acute kidney injury?
It depends. If AKI is caused by dehydration or low blood flow, IV fluids can help. But if it’s from heart failure or fluid overload, drinking more water can make it worse. Never self-treat with fluids if you have swelling, shortness of breath, or are on dialysis. Always follow medical advice.
Is acute kidney injury the same as chronic kidney disease?
No. AKI is sudden and often reversible. Chronic kidney disease (CKD) is gradual damage that lasts longer than three months. But AKI can lead to CKD. About 23% of AKI survivors develop stage 3 or worse CKD within a year. Each episode increases your long-term risk of needing dialysis.
What Comes After Recovery?
Recovery isn’t the end-it’s the start of a new routine. Forty-five percent of AKI survivors need to see a nephrologist within six months. Your kidneys may look fine on paper, but they’ve been through trauma. They need protection.
Follow-up blood tests every 3-6 months. Avoid NSAIDs. Control blood pressure and blood sugar. Stay hydrated. Eat less salt. These aren’t suggestions-they’re lifelines.
AKI is a wake-up call. It’s not just about kidneys. It’s about your whole body. And the next time you feel tired, swollen, or just “off”-ask yourself: Could this be my kidneys trying to tell me something?


i literally just had my grandma go through this last year. she thought she was just 'feeling old' until she passed out in the kitchen. turned out her creatinine was through the roof. she's fine now, but man, this post hit home.
January 27don't ignore fatigue. it's not just aging.
Kathy McDaniel