You give your child amoxicillin for an ear infection. Three days in, a pink, spotty rash appears on their chest and arms. Panic sets in. Is this an allergic reaction? Should you stop the medicine? What if it’s something worse? You’re not alone. Nearly one in five parents stop antibiotics at the first sign of a rash - and most of the time, they’re wrong.
Most Antibiotic Rashes Aren’t Allergies
Let’s clear up the biggest myth right away: most rashes from antibiotics, especially amoxicillin, are not allergic reactions. In fact, up to 90% of kids labeled as allergic to amoxicillin because of a rash turn out to be perfectly fine when tested. The rash isn’t your body fighting the drug - it’s often your body fighting a virus.Here’s the science: if your child has a viral infection like Epstein-Barr (mono) or a common cold, and you give them amoxicillin, their immune system can react to the drug in a harmless way. The result? A flat, pink, patchy rash that looks like tiny bruises. It usually shows up between days 5 and 10 of treatment. It doesn’t itch much. It doesn’t move around. And it doesn’t mean your child is allergic.
True allergic reactions? Those are different. They happen fast - within an hour of taking the drug. The rash looks like raised, red, itchy welts (hives). It might swell the lips or tongue. Breathing could get hard. That’s when you stop the medicine and act.
How to Tell the Difference
Knowing what to look for can save you from unnecessary panic - and from making things worse.- Non-allergic rash (most common): Appears 5-10 days after starting the antibiotic. Flat, pink spots. Mostly on the trunk, arms, or legs. Not itchy. Doesn’t change shape or move. Your child feels fine - no fever, no trouble breathing, no sore throat.
- Allergic rash (true allergy): Comes on fast - within minutes to an hour. Raised, red, itchy bumps (like hives). May swell. Could cause vomiting, wheezing, or dizziness. This is serious.
- Severe reaction (rare but dangerous): Rash with blisters, peeling skin, mouth sores, high fever (over 38.5°C), swollen lymph nodes. This could be Stevens-Johnson Syndrome or DRESS syndrome. Requires emergency care.
Don’t rely on how scary it looks. A mild-looking rash can be dangerous. A scary-looking one might be harmless. Focus on timing, shape, and symptoms.
When to Keep Taking the Antibiotic
If the rash is flat, not itchy, and appears after day 5 - keep giving the antibiotic. Yes, really.Stopping it unnecessarily does more harm than good. The CDC found that patients wrongly labeled as allergic get worse antibiotics more often - ones that are broader, cost more, and cause more side effects. In kids, stopping amoxicillin for a harmless rash leads to:
- 37% higher chance the infection comes back
- 28% more need for stronger antibiotics like clindamycin
- 63% higher risk of severe diarrhea from C. diff
One mom on Reddit shared: “I stopped amoxicillin because of the rash. Two days later, the ear infection was worse. We had to switch to clindamycin. My kid had diarrhea for two weeks.” That’s avoidable.
Doctors in pediatric clinics across the U.S. and U.K. now agree: if the rash fits the non-allergic pattern, continue the course. The rash will fade on its own in 5-7 days. No treatment needed.

When to Stop the Antibiotic and Call the Doctor
Now, here’s when you must stop:- Rash appears within 1 hour of taking the drug
- Rash is raised, bumpy, and extremely itchy
- Swelling of the face, lips, or tongue
- Difficulty breathing, wheezing, or tightness in the throat
- Fever over 38.5°C
- Blisters, peeling skin, or sores in the mouth or eyes
If any of these happen, stop the antibiotic immediately. Call your doctor or go to urgent care. If breathing is affected, call emergency services. Don’t wait.
For mild allergic reactions (hives without breathing trouble), you can give an antihistamine like cetirizine (Zyrtec) - but still call your doctor. For severe reactions, epinephrine may be needed. Hospitals have protocols for this. Don’t try to handle it alone.
What to Do While Waiting for the Doctor
If you’re unsure, don’t guess. Here’s what works:- Take a photo. Skin changes fast. A photo helps the doctor see what you saw.
- Write down the timing. When did the rash start? After which dose? What else was happening that day?
- Don’t give new meds. No extra antihistamines, no steroid creams unless told to. You might mask symptoms.
- Don’t panic. Most rashes are harmless. But don’t ignore warning signs.
Many parents try to treat the rash with hydrocortisone cream or Benadryl. That’s fine for itching - but it won’t make the rash go away faster. And it won’t change whether it’s allergic or not. The only thing that matters is whether the drug is safe to keep taking.
Why Mislabeling Matters
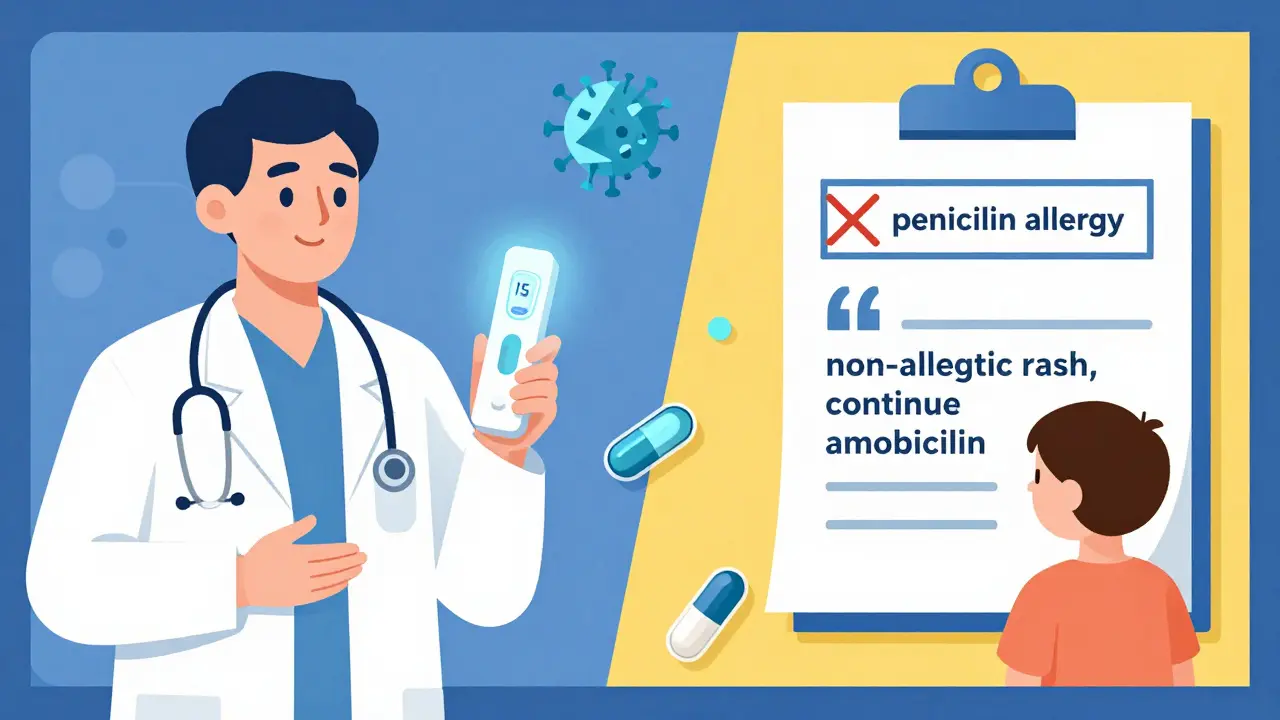
Calling your child “allergic to penicillin” because of a rash can follow them for life. That label gets added to their medical record. It affects every future infection.Here’s what happens:
- Doctors avoid penicillin-like drugs - even if they’re the best choice
- They pick stronger, broader-spectrum antibiotics
- Those drugs cost more, cause more diarrhea, and increase the risk of superbugs like C. diff
- Studies show patients with false penicillin labels have a 30% higher risk of dying from sepsis
The CDC estimates that mislabeling costs the U.S. healthcare system $1.2 billion a year. In the U.K., the same problem exists - with fewer resources to test and correct it. That’s why accurate diagnosis isn’t just about comfort - it’s about survival.
What’s New in 2026
Things are improving. In 2023, the FDA approved a new rapid test called PENtest - it gives results in 15 minutes instead of 3 hours. More clinics are using it. AI tools are being tested too. One app, still in trials, can analyze a rash photo and tell you with 89% accuracy whether it’s likely allergic or not.But the biggest change? Doctors are finally teaching parents how to spot the difference. The American Academy of Pediatrics now includes clear guidelines in patient handouts. Hospitals are training nurses to explain rashes before discharge.
Still, only 38% of family doctors feel confident telling the difference. That’s why you need to know this too.
Bottom Line: What to Remember
- If the rash is flat, appears after day 5, and your child feels fine - keep giving the antibiotic.
- If the rash is bumpy, itchy, comes on fast, or you see swelling or trouble breathing - stop the drug and call your doctor or go to urgent care.
- Don’t call it an allergy unless a doctor confirms it.
- Document the rash accurately: “maculopapular rash on trunk, non-itchy, day 7 of amoxicillin” - not “allergic to penicillin.”
Antibiotics save lives. A harmless rash shouldn’t stop them. But a real allergic reaction? That’s an emergency. Learn the difference. Trust your instincts - but don’t let fear make the decision for you.
Is it safe to keep giving amoxicillin if my child has a rash?
Yes - if the rash is flat, pink, appears after day 5 of treatment, and your child has no fever, trouble breathing, or swelling. This is a common non-allergic reaction, especially with viral infections. Stopping the antibiotic unnecessarily increases the risk of the infection returning or requiring stronger, riskier drugs. Always check with your doctor, but in most cases, continuing is the safest choice.
How long does an antibiotic rash last?
Non-allergic rashes usually last 5 to 10 days and fade on their own after you finish the antibiotic. They don’t get worse with time. True allergic rashes (hives) can come and go within hours, but if they persist beyond a day or two, it may signal a more serious reaction. Severe rashes like Stevens-Johnson Syndrome require hospital care and can last weeks.
Can I give my child antihistamines for the rash?
If the rash is itchy and you’re sure it’s not a severe reaction, you can give an antihistamine like cetirizine (Zyrtec) - but only after checking with your doctor. For non-allergic rashes, antihistamines don’t speed up healing - they just help with itching. For true allergic reactions, antihistamines are part of first aid, but they’re not enough on their own. Never use them to mask symptoms and continue the antibiotic if you suspect a real allergy.
Should I get my child tested for penicillin allergy?
If your child had a rash while on amoxicillin and you’re unsure whether it was an allergy, yes - testing is safe and highly recommended. Skin tests and oral challenges are accurate, low-risk, and can clear up false labels. The CDC estimates 92% of people labeled as allergic to penicillin tolerate it when tested. Testing is now faster than ever, with rapid tests available in many clinics.
What’s the difference between a rash from amoxicillin and one from other antibiotics?
Amoxicillin is the most common cause of non-allergic rashes - especially in kids with viral infections. Other antibiotics like sulfa drugs or vancomycin are more likely to cause true allergic reactions. But the rash itself doesn’t tell you the drug - timing and appearance do. A flat, non-itchy rash after day 5? Likely amoxicillin. Raised, itchy rash within an hour? Could be any antibiotic. Always report the exact drug name to your doctor.