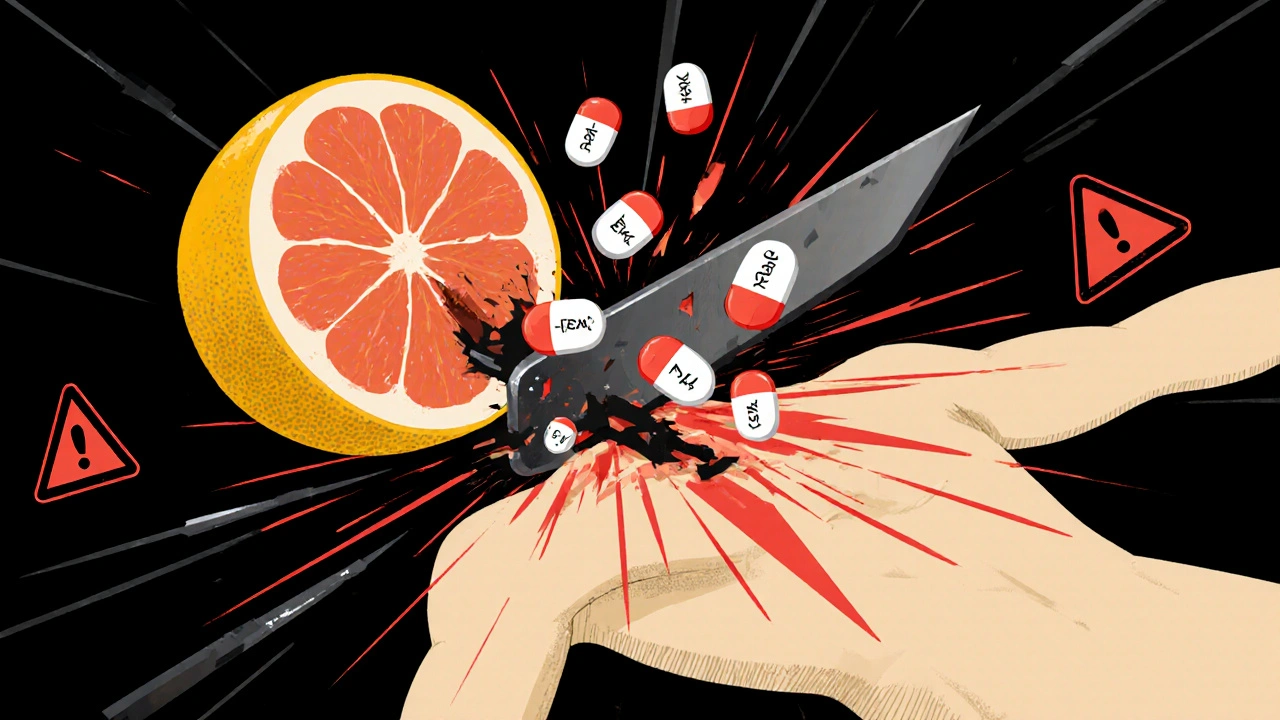
Drinking a glass of grapefruit juice in the morning might feel like a healthy habit-until it puts your life at risk. If you’re taking certain medications, that refreshing citrus sip could be turning your pills into a dangerous overdose. This isn’t a myth. It’s not a warning you can ignore. And it’s not something that only happens if you drink a whole pitcher. Just one glass of grapefruit juice can change how your body handles your medicine-sometimes for days.
Why Grapefruit Juice Changes How Your Medicines Work
Grapefruit juice doesn’t just mix poorly with some drugs. It actively breaks down a key system in your body that’s meant to protect you from too much medication. That system is called CYP3A4, an enzyme in your intestines that breaks down about half of all oral drugs before they enter your bloodstream. Think of it like a gatekeeper. It lets in just enough of the drug to work, then stops the rest from flooding your system. Grapefruit juice shuts down that gatekeeper. It contains chemicals called furanocoumarins-mainly bergamottin and 6',7'-dihydroxybergamottin-that permanently disable CYP3A4 enzymes. Once they’re knocked out, your body can’t break down the drug properly. So instead of 10% of the drug entering your blood, it might be 50%, 100%, or even 800%. That’s not a small bump. That’s a spike into dangerous territory. The worst part? This isn’t temporary. One 200-milliliter glass (about 6.7 ounces) can reduce CYP3A4 activity by 47% within four hours. And because your body needs to make new enzymes to replace the damaged ones, the effect lasts 24 to 72 hours. That means even if you take your pill at night and drink grapefruit juice in the morning, you’re still at risk.Which Medications Are Most at Risk?
More than 85 prescription drugs in the U.S. and Canada are known to interact with grapefruit juice. Of those, 43 can cause life-threatening reactions. Here’s what you need to watch for:- Statins (cholesterol drugs): Simvastatin (Zocor) is the most dangerous. Just one glass of grapefruit juice can triple your blood levels. That raises your risk of rhabdomyolysis-a condition where muscle tissue breaks down and can lead to kidney failure. Atorvastatin (Lipitor) is less affected, but still risky. Pravastatin and rosuvastatin? Safe. No interaction.
- Calcium channel blockers (blood pressure meds): Felodipine (Plendil) sees a 5-fold increase in blood levels. Nifedipine (Procardia) jumps 3.3 times. Amlodipine (Norvasc)? Minimal effect. If you’re on blood pressure meds, know which one you’re taking.
- Immunosuppressants: Cyclosporine (Neoral), used after transplants, can spike 50-60% in concentration. That can cause kidney damage. Tacrolimus is a safer alternative.
- Antiarrhythmics: Amiodarone (Cordarone) levels rise 30-40%, increasing the risk of irregular heart rhythms that can be fatal.
- Others: Some sedatives like triazolam, certain pain meds like fentanyl, and even some antidepressants like sertraline can be affected.
On the flip side, some medications show little to no interaction. Trazodone, zolpidem, and levothyroxine are generally safe. But here’s the catch: you can’t assume. Always check with your doctor or pharmacist.
Not All Citrus Is the Same
You might think, “If grapefruit is bad, what about oranges or lemons?” Not all citrus fruits are created equal. Seville oranges (used in traditional marmalade) and pomelos contain the same dangerous furanocoumarins. So if you’re on a risky medication, skip those too. Sweet oranges (like navel or Valencia), tangerines, and lemons? Safe. They don’t contain the chemicals that disable CYP3A4. So you can still enjoy your morning orange juice-just not the grapefruit kind.
Why This Interaction Is So Hard to Predict
You might wonder: “Why do some people get hit hard and others don’t?” The answer is biology. People naturally have different levels of CYP3A4 in their intestines. Someone with high baseline enzyme activity will see a massive spike in drug levels after grapefruit. Someone with low levels? Maybe barely a change. A 2013 study showed that after drinking 250mL of grapefruit juice, one person’s felodipine levels jumped 8-fold compared to water. Another person’s? No change at all. There’s no blood test to tell you where you fall. And you can’t guess based on age, weight, or health. That’s why experts say the only safe rule is: if your drug interacts with grapefruit, avoid it completely.What You Should Do Right Now
If you’re taking any prescription medication, here’s your action plan:- Check your medication label. Since 2014, the FDA requires manufacturers to warn about grapefruit interactions on the prescribing information. Look for phrases like “avoid grapefruit juice” or “do not consume grapefruit products.”
- Ask your pharmacist. They’re trained to spot these interactions. A 2021 study found 89% of community pharmacists routinely screen for grapefruit when dispensing meds.
- Keep a full list of everything you take-not just prescriptions, but supplements and over-the-counter drugs too. Fexofenadine (Allegra), an antihistamine, can also be affected.
- If you’re on a high-risk drug like simvastatin or cyclosporine, talk to your doctor about switching to a safer alternative. Pravastatin instead of simvastatin. Tacrolimus instead of cyclosporine. These swaps can eliminate the risk entirely.
- Don’t wait for symptoms. Toxic levels build up silently. You might feel fine until your muscles start failing or your heart goes out of rhythm.
Who’s Most at Risk?
Older adults are the most vulnerable group. People over 65 make up 40% of grapefruit juice drinkers in the U.S., according to USDA data. They’re also more likely to be on 3-5 medications at once-many of which interact with grapefruit. That’s a perfect storm. The American Geriatrics Society specifically warns seniors to be extra careful. But it’s not just seniors. Anyone on long-term meds for heart disease, high cholesterol, or organ transplants needs to pay attention.What’s Changing in the Future?
The good news? Science is catching up. In October 2023, the USDA announced that CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety trials. These aren’t on shelves yet, but they’re a sign that the problem is being solved at the source. Regulators are also stepping up. The European Medicines Agency now requires all new oral drugs metabolized by CYP3A4 to be tested for grapefruit interactions. The FDA updated its guidance in 2020 to make sure drug makers test with 200mL of juice under fasting conditions-the real-world scenario that causes the worst reactions. But until those safer grapefruits hit the market, the rule stays simple: if your medicine has a grapefruit warning, don’t take the risk.What Happens If You Accidentally Drink It?
If you had a glass of grapefruit juice and later realized your medication interacts with it, don’t panic-but don’t ignore it either. - If you’re on a high-risk drug like simvastatin or cyclosporine, call your doctor. They may want to check your kidney or liver function, or monitor your heart rhythm. - If you’re on a lower-risk drug like atorvastatin, monitor for unusual side effects: muscle pain, weakness, dark urine, dizziness, or irregular heartbeat. - Don’t skip your next dose. Just avoid grapefruit from now on. The key is awareness. Most people don’t know about this interaction. A 2022 survey found only 38% of patients recalled being warned about grapefruit when prescribed a risky medication. Don’t be one of them.Can I drink grapefruit juice if I take my medication at a different time of day?
No. The effect of grapefruit juice lasts 24 to 72 hours after you drink it. Even if you take your pill at night and drink juice in the morning, your body still won’t be able to break down the drug properly. The interaction isn’t about timing-it’s about whether the enzyme system is working at all. Avoid grapefruit entirely while on affected medications.
Is grapefruit juice the only problem, or do whole grapefruits count too?
Whole grapefruit has the same effect as the juice. The furanocoumarins are in the pulp and peel, not just the liquid. Eating a grapefruit or even a section of it can trigger the same dangerous interaction. Don’t assume juicing makes it worse-eating it is just as risky.
What about grapefruit-flavored sodas or candy?
Most grapefruit-flavored sodas, candies, or snacks use artificial flavoring and don’t contain real grapefruit or furanocoumarins. They’re generally safe. But always check the ingredient list. If it says “grapefruit juice concentrate” or “natural grapefruit flavor,” it could still be risky. When in doubt, avoid it.
Can I drink grapefruit juice if I’m not on any medication?
Yes. Grapefruit juice is perfectly safe if you’re not taking any drugs that interact with it. It’s a good source of vitamin C and antioxidants. The danger only exists when it’s mixed with certain medications. If you’re unsure whether your meds are affected, check with your doctor or pharmacist before drinking it.
Are there any new drugs that don’t interact with grapefruit?
Yes. Many newer medications are designed to avoid CYP3A4 metabolism entirely. For example, pravastatin and rosuvastatin (statins), amlodipine (blood pressure), and levothyroxine (thyroid) don’t interact with grapefruit. Drug manufacturers are now required to test for these interactions during development, so newer drugs are less likely to have this problem. But always verify-never assume.




Okay but have you ever considered that maybe the real problem isn't grapefruit juice-it's our entire fucking pharmaceutical system? We're told to take pills like they're candy, then get mad when nature fights back. Grapefruit just exposes how lazy we are about our own bodies. You don't need a warning label-you need to ask why your body can't handle the dose in the first place.
November 26katia dagenais