Every year, millions of people in the U.S. are prescribed opioids for pain. For some, it’s a short-term solution after surgery or injury. For others, it becomes a long-term reality. But the cost of that relief can be devastating. In the 12 months ending June 2025, over 108,300 people died from drug overdoses-86% of them involving synthetic opioids. That’s not just a statistic. It’s a crisis that’s reshaping how doctors prescribe pain medicine.
Why Opioids Are Riskier Than You Think
Opioids work by binding to receptors in your brain to block pain signals. They’re effective-sometimes the only thing that works for severe pain. But they also trigger dopamine release, which creates euphoria. That’s why they’re addictive. The risk isn’t just about taking too much. It’s about how long you take them. According to the CDC’s 2025 guidelines, patients taking more than 50 morphine milligram equivalents (MME) per day are nearly three times more likely to overdose than those on lower doses. And for every extra 20 MME above that threshold, the risk of overdose climbs by 1.7 times. That’s not a guess. It’s based on data from over 2 million patients tracked from 2022 to 2024. Even more concerning: 12.7% of people on long-term opioid therapy develop moderate-to-severe opioid use disorder (OUD), according to FDA studies published in July 2025. That means nearly 1 in 8 patients prescribed opioids for chronic pain will struggle with addiction. And many don’t realize it until it’s too late.The New Rules for Prescribing Opioids
In 2025, the rules changed. The CDC, FDA, and CMS all updated their guidelines to reduce harm without cutting off access to care. Here’s what matters now:- Three-day limit for acute pain: For injuries, dental work, or post-surgery pain, the default prescription is now three days. Only if your doctor has clear evidence you’ll need more-like a major surgery or complex fracture-can they extend it to seven days.
- 90 MME is a hard stop: Prescribing more than 90 MME per day is strongly discouraged unless you’re in cancer care, palliative care, or end-of-life treatment. Any prescription above that requires detailed documentation and justification.
- Point-of-sale safety edits: Starting January 2025, pharmacies must block initial opioid prescriptions that exceed three days or push a patient past 90 MME per day. This isn’t optional. It’s built into the pharmacy’s computer system.
What Doctors Are Doing Differently
Clinicians aren’t just writing fewer scripts. They’re changing how they think about pain. Many now use risk assessment tools like the Opioid Risk Tool (ORT) or SOAPP before prescribing. A score below 4 means low risk-standard monitoring applies. A score of 4 to 7 means moderate risk: more frequent check-ins, urine tests, and a push toward non-opioid options. A score above 8? That’s high risk. Most doctors won’t prescribe opioids at all without a specialist’s input. They’re also checking Prescription Drug Monitoring Programs (PDMPs) before writing a script. That’s a state database that shows what other medications a patient has been prescribed. Studies show checking PDMPs reduces dangerous overlapping prescriptions by 37%. It adds about 2.5 minutes per visit-but it saves lives. And they’re asking different questions. Instead of “How bad is your pain?” they’re asking “What have you tried already?” and “Have you ever struggled with substance use?”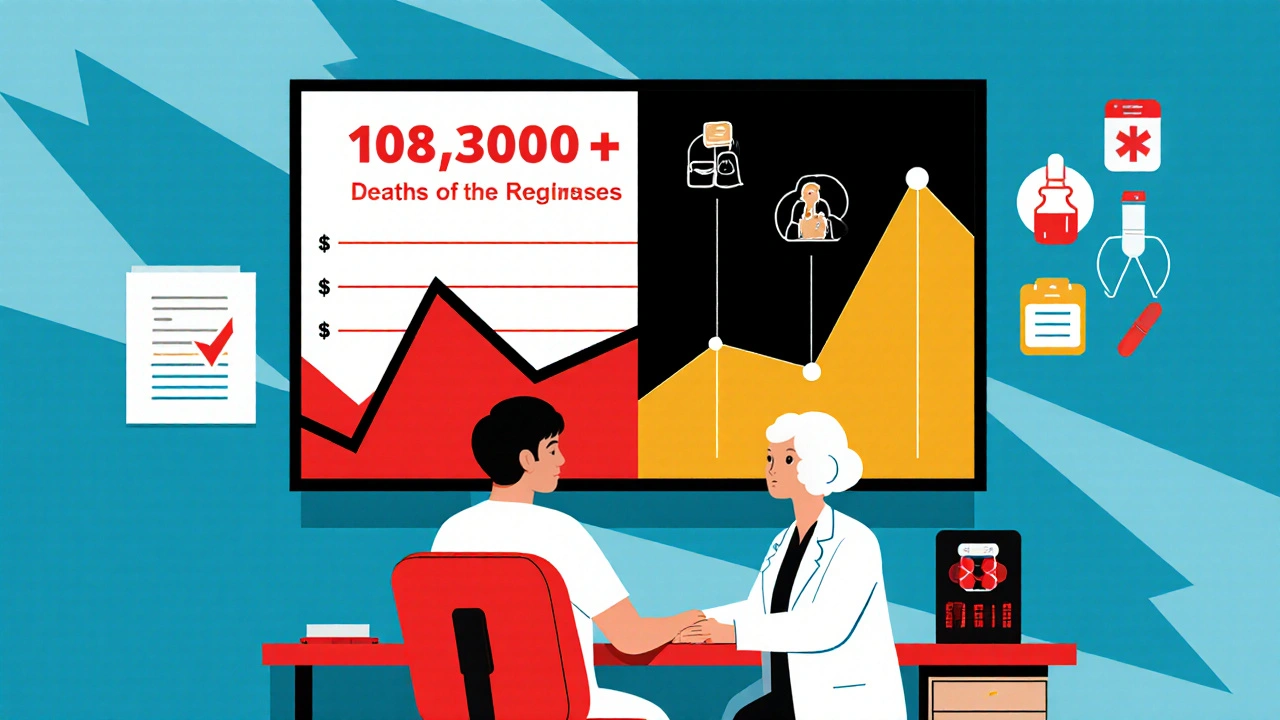
Non-Opioid Alternatives That Actually Work
The biggest shift in pain management isn’t about opioids. It’s about what comes before them.- NSAIDs (like ibuprofen or naproxen) are now first-line for most types of acute and chronic pain. They’re cheaper, safer, and just as effective for many conditions.
- Acetaminophen remains a cornerstone for mild-to-moderate pain, especially when combined with other therapies.
- Physical therapy is proven to reduce opioid use by 40-50% in patients with back pain, arthritis, or post-surgical recovery.
- Cognitive behavioral therapy (CBT) helps patients manage pain perception, reduce anxiety around pain, and improve function without drugs.
- CBD-based products are gaining traction. While not FDA-approved for pain, early data shows promise for nerve pain and inflammation with minimal risk of addiction.
The Hidden Cost of Overly Strict Rules
It’s not all progress. Some patients are getting caught in the crossfire. Dr. Michael Chen, a primary care doctor in Ohio, says his three-day limit for acute pain cut new long-term opioid use by 35%. But he’s also had 12 patients show up in the ER because their pain returned after their prescription ran out. The U.S. Pain Foundation surveyed 1,200 chronic pain patients in 2025 and found that 7-10% had their opioids abruptly stopped-sometimes without a plan. That led to severe withdrawal, increased pain, and even suicide attempts. The FDA’s 2025 warning is clear: never taper opioids too fast. Sudden discontinuation can be deadly. And for veterans with PTSD or trauma-related pain, the VA’s Opioid Safety Initiative has helped. But it’s not available everywhere. Rural clinics often lack the staff, training, or resources to implement these complex protocols.
What You Should Do If You’re on Opioids
If you’re taking opioids for pain, here’s what to ask your doctor:- “What’s my current MME dose?” (Ask them to calculate it. Many patients don’t know.)
- “Have you checked my PDMP record?”
- “What non-opioid options have we tried?”
- “Is there a plan to reduce my dose over time?”
- “What happens if I need more than three days for acute pain?”
The Bigger Picture: Where We’re Headed
By 2027, experts predict 65% of acute pain episodes will be managed without opioids. That’s up from 48% in 2025. The driving force? Multimodal care-combining physical therapy, counseling, NSAIDs, and targeted nerve blocks. The NIH has invested $125 million into developing non-addictive pain treatments. New drugs are in trials. Insurance companies are starting to cover more non-opioid therapies. And states are tightening rules: 38 now cap acute opioid prescriptions at 3 to 7 days. But there’s a bottleneck: a shortage of 12,500 pain specialists. Rural areas are hit hardest. Sixty-eight percent of rural counties don’t have a dedicated pain clinic. The challenge isn’t just medical. It’s systemic. We need more training for primary care doctors. More funding for community-based pain programs. Better integration of mental health services. And above all, we need to treat pain as a whole-person issue-not just a number on a scale.Final Thought: Balance Is Everything
The goal isn’t to ban opioids. It’s to use them wisely. For someone with terminal cancer, opioids can mean dignity in their final days. For someone with a broken ankle, they might mean a few days of relief while healing. But for millions of others-people with chronic back pain, arthritis, or fibromyalgia-there are safer, more sustainable paths. The science is clear. The tools exist. What’s missing is the will to use them. The next time you or someone you care about is prescribed opioids, ask: Is this truly necessary? What else can we try? And how do we get off this path safely if we don’t need it?What is the maximum safe opioid dose per day in 2025?
According to the 2025 CDC and FDA guidelines, doses above 90 morphine milligram equivalents (MME) per day should be avoided unless the patient has cancer, is in palliative care, or is at end-of-life. Even then, careful documentation and specialist oversight are required. Doses above 50 MME per day are considered high risk, with a 2.8 times higher chance of overdose compared to lower doses.
Can I still get a 7-day opioid prescription for acute pain?
Yes-but only if your doctor provides clear clinical justification. The default is now three days for most acute pain, like after dental work or minor surgery. A seven-day supply is allowed only in cases like major trauma, complex fractures, or surgeries where recovery is known to take longer. Pharmacists are required to block prescriptions that exceed this unless properly documented.
Do I need to get my prescription checked through a drug monitoring program?
Yes. Most states now require doctors to check the Prescription Drug Monitoring Program (PDMP) before prescribing opioids. This helps prevent dangerous combinations and overlapping prescriptions. While it adds a few minutes to your appointment, it’s a critical safety step. Studies show this practice reduces risky prescribing by 37%.
What are the safest alternatives to opioids for chronic pain?
The most effective non-opioid options include NSAIDs (like ibuprofen), acetaminophen, physical therapy, cognitive behavioral therapy (CBT), and certain nerve-targeted treatments like TENS units. CBD-based products are also being studied and used off-label with promising results for nerve pain and inflammation. Practices that combine these approaches see up to 50% lower opioid use without worsening pain control.
What should I do if my doctor wants to taper my opioid dose?
Never stop opioids suddenly. Ask your doctor for a slow, personalized taper plan-usually reducing by 10% every 1-2 weeks. Rapid tapering increases the risk of severe withdrawal, uncontrolled pain, and even suicide. If your doctor pushes for a fast taper without a plan, seek a second opinion. The FDA explicitly warns against abrupt discontinuation for this reason.
Are there any new pain medications coming soon?
Yes. The NIH has allocated $125 million for non-addictive pain therapies through its HEAL Initiative. Several new drugs targeting nerve pain and inflammation without opioid receptors are in late-stage trials. These include novel non-opioid analgesics and targeted biologics. Experts expect the first wave of these to become available between 2027 and 2029, potentially replacing opioids for many chronic conditions.
If you’re managing chronic pain, remember: you’re not alone. The system is changing. And you have more options than you think. Talk to your doctor. Ask questions. Push for alternatives. Your safety is worth it.





Man, I’ve been on opioids for my back for years and this article actually gave me hope. I didn’t realize how much safer stuff like PT and CBT could be-my doc never even mentioned them. Just started physical therapy last month and my pain’s down 30%. No more daily pills. Feels like I got my life back.
November 26Also, the 90 MME cap? Long overdue. My cousin overdosed last year at 120 MME. They didn’t even know they were that high. We need more awareness, not just rules.
Joe bailey