If you’re dealing with migraine 15 or more days a month, you’ve probably tried pills, patches, and lifestyle changes. Maybe they helped a little. Maybe they made you feel worse. There’s another option that doesn’t involve swallowing something daily - and it’s been helping thousands of people for over a decade: Botox injections.
It sounds surprising. Botox? The same thing people use to smooth forehead wrinkles? But for chronic migraine, it’s not about looking younger. It’s about stopping the pain before it starts.
How Botox Actually Stops Migraines
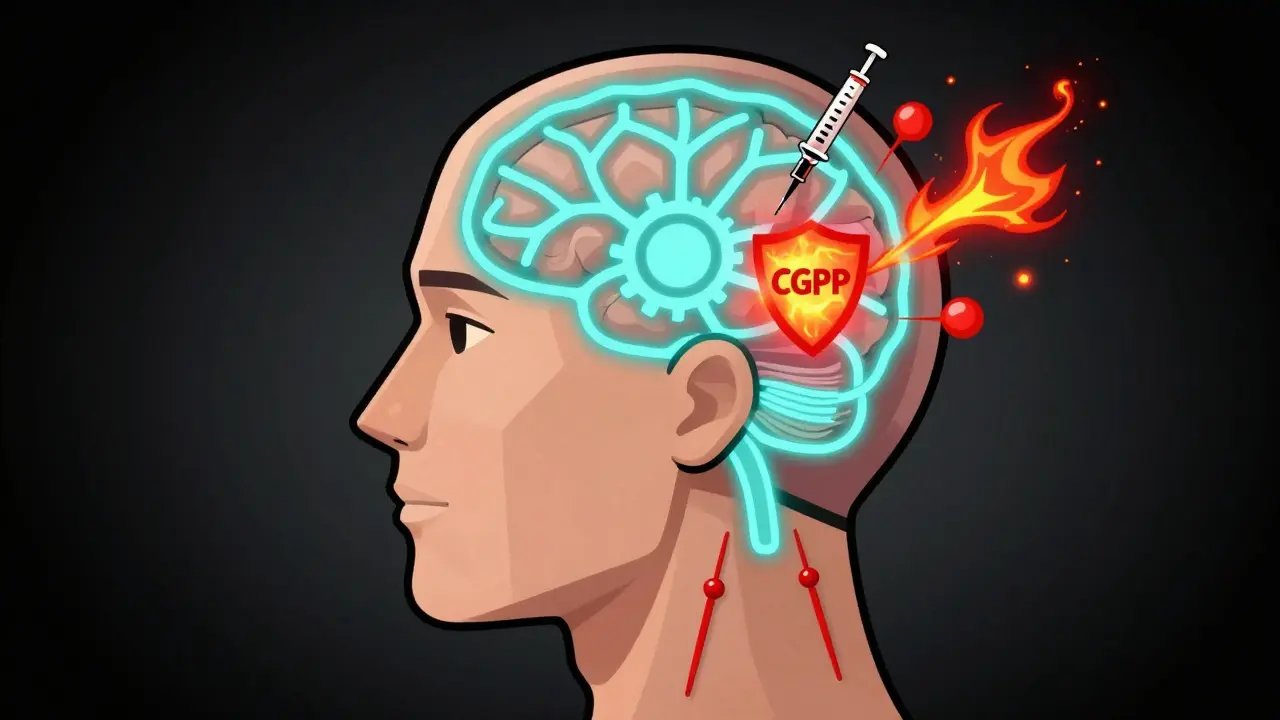
Botox isn’t just a muscle relaxer. That’s the myth. The real science is deeper. The active ingredient, onabotulinumtoxinA, blocks the release of chemicals that trigger pain signals in your nerves. Specifically, it stops something called CGRP - calcitonin gene-related peptide - from flooding your system during a migraine attack. CGRP is like a fire alarm for your brain. When it’s turned up too high, you get the pounding headache, nausea, light sensitivity - the whole package.
These injections don’t just sit in your skin. They travel slightly along nerve pathways, targeting the trigeminal nerve, which is the main pain highway for migraines. By quieting the nerve endings in your head and neck, Botox reduces both the frequency and intensity of attacks. It doesn’t numb you. It doesn’t make you sleepy. It just turns down the volume on the pain signals.
Studies show it works on the nervous system in three ways: it reduces inflammation around nerves, blocks pain signals from reaching your brain, and helps calm the brain’s sensitivity over time. This last part is key. Chronic migraine isn’t just bad days - it’s your brain becoming wired to hurt more easily. Botox helps rewire that.
Who Gets the Most Out of Botox?
Not everyone with headaches qualifies. Botox is FDA-approved only for chronic migraine, which means 15 or more headache days a month, with at least eight of them having migraine features like throbbing pain, nausea, or sensitivity to light and sound.
If you have fewer than 15 headache days a month - what’s called episodic migraine - Botox won’t help. Clinical trials proved that. It’s not a one-size-fits-all fix.
The people who benefit most are those who’ve tried at least three other preventive medications - things like topiramate, propranolol, or amitriptyline - and couldn’t stick with them because of side effects. Fatigue, brain fog, weight gain, tingling hands - those are common reasons people quit oral drugs. Botox avoids those entirely.
It’s also especially helpful if you have medication-overuse headache. That’s when you’re taking painkillers too often - more than 10 days a month - and they start making your headaches worse. Botox can break that cycle.
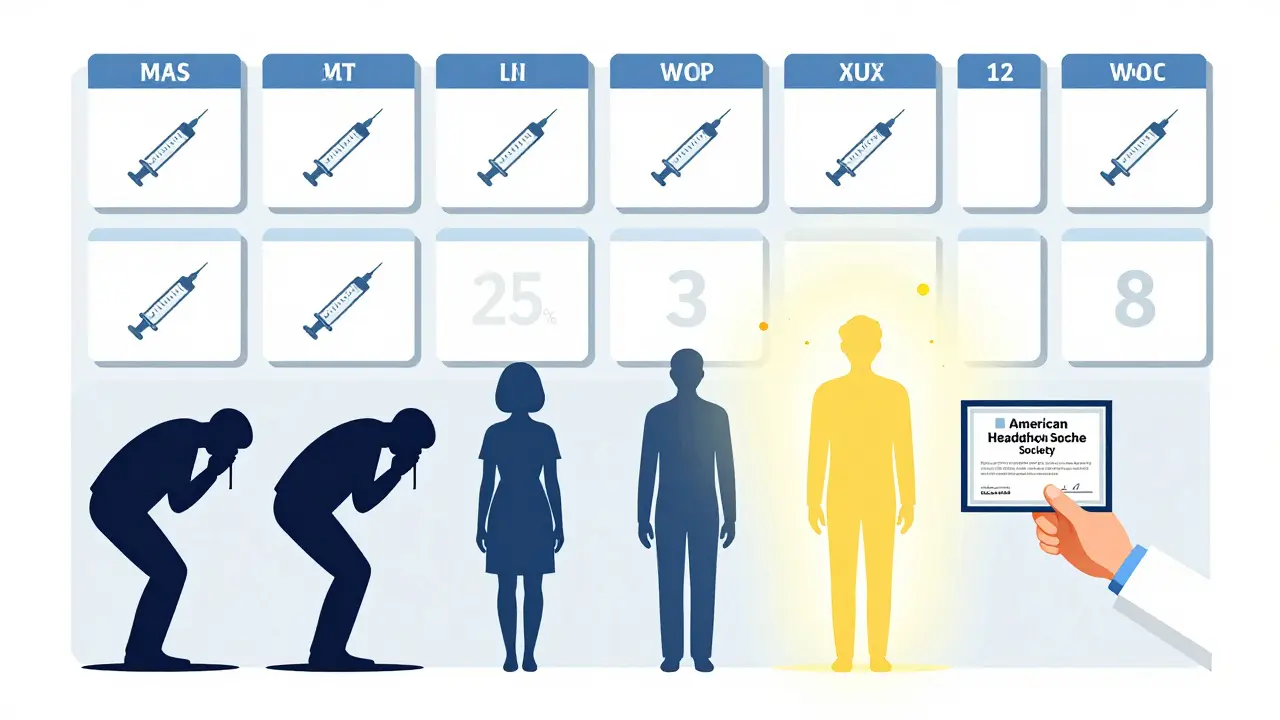
Real-world data from over 1,200 patients showed that 63% cut their headache days by half or more after one year. For some, it went from 25 days a month down to 8. Others saw their worst migraines go from debilitating to manageable. It’s not a cure, but it’s a game-changer for those stuck in the cycle.
What the Treatment Actually Looks Like
Getting Botox for migraine isn’t a quick poke. It’s a precise procedure based on the PREEMPT protocol. That means 31 to 39 tiny injections across seven specific spots: your forehead, between your eyebrows, your temples, the back of your head, and your neck and shoulders. The whole thing takes about 15 minutes. No anesthesia. Just a small needle.
You might feel a pinch. Some people get a mild headache right after. A few report temporary neck weakness or a droopy eyelid - but that’s rare, happening in under 4% of cases. Most people walk out the door and go back to work.
The injections are given every 12 weeks. That’s every three months. It’s not something you do once and forget. You need to stick with it. Most people don’t feel the full effect until their third or fourth round. That’s normal. Your body needs time to respond.
Only neurologists or headache specialists trained in the PREEMPT method should give these injections. There’s a reason. Studies show injector experience affects outcomes by up to 30%. A poorly placed injection won’t help - and might even cause discomfort. Make sure your provider has done the American Headache Society’s certification course.
How It Compares to Other Treatments
Let’s say you’re comparing options. Here’s how Botox stacks up:
- Topiramate: Works for many, but causes brain fog, memory issues, and tingling. About 35% of people quit because of side effects.
- Propranolol: Lowers blood pressure. Can make you tired or dizzy. Not good for people with asthma or low heart rate.
- CGRP antibodies (like Aimovig, Emgality): Newer, injectable monthly shots. Slightly more effective than Botox, but cost is higher - and they’re not covered by all insurance.
- Botox: No daily pills. No systemic side effects. No liver or kidney stress. Just a few shots every 3 months.
Response rates? About 47% of Botox patients cut their headache days by half. That’s better than propranolol and topiramate. It’s close to the newer CGRP drugs, which hit around 52%. But Botox has a decade of safety data behind it. The newer drugs? We’re still watching long-term effects.
And here’s something important: Botox and CGRP drugs can be used together. Recent studies show combining them boosts results. Patients who tried both had a 68% response rate - better than either alone.
Cost, Insurance, and Real-Life Hurdles
One shot of Botox for migraine costs between $1,500 and $1,800. That’s $6,000 to $7,200 a year. Sounds steep. But here’s the catch: most insurance plans cover it - if you meet the criteria.
Insurance companies want proof you’ve tried and failed at least three other preventives. They usually require 3 months of headache diaries. That’s not optional. You need to track your days, symptoms, and triggers.
One patient in Seattle told me she spent 8 months fighting her insurer. Denied twice. Finally approved after her doctor submitted detailed records and a letter explaining her medication-overuse headache. It took time, but it worked.
Some clinics offer payment plans. AbbVie (the maker of Botox) has a patient assistance program for those without insurance or with high copays. It’s worth asking.
Don’t let cost scare you off. Think about this: if you’re missing 10 days a month of work, family time, or just normal life, how much is that really costing you? Botox isn’t just medicine. It’s time back.
What Patients Really Say
On forums like Migraine.com and Reddit, people are honest. One user wrote: “After three rounds, I went from 25 migraine days a month to 8-10. My worst ones are now just bad, not ‘call 911’ bad.”
Others say: “I don’t need triptans as often.” “I can finally plan a weekend.” “My kids don’t have to tiptoe around me anymore.”
But it’s not perfect. Some say: “The injections hurt.” “My neck felt weird for a week.” “Insurance denied me again.” “I didn’t feel anything after the first two rounds.”
That’s normal. Not everyone responds. About 20% don’t see a big change. But for those who do - it’s life-changing. The key is patience and persistence.
What’s New in 2025
Botox for migraine isn’t standing still. In June 2023, the FDA approved it for teens aged 12 to 17 with chronic migraine. That’s huge. For the first time, adolescents have a proven, non-pill option.
Researchers are also testing longer-lasting versions. One experimental formula could last 16 to 20 weeks instead of 12. That means fewer visits. Less disruption. More consistency.
And scientists are starting to match Botox to patient types. Not all chronic migraine is the same. Some have neck tension. Others have light sensitivity. Some have digestive issues. The goal now isn’t just “does it work?” - it’s “who does it work best for?”
One study in Copenhagen found patients with neck pain and muscle tightness responded better than those without. That’s the future: personalized treatment.
Final Thoughts
Botox for migraine isn’t magic. It’s medicine - backed by solid science, real patient results, and years of use. It’s not for everyone. But if you’re stuck in a loop of daily pain, failed pills, and insurance battles, it might be the break you’ve been waiting for.
It won’t erase every headache. But it can turn your life from surviving to living. And that’s worth more than a few shots every three months.





So Botox isn't just for wrinkles anymore? I mean, I get it - if your brain’s screaming every day, you’ll try anything. But still… I picture someone sitting in a chair, getting tiny needles in their scalp like a human pin cushion, and just… waiting for the pain to shut up. Kinda poetic, in a weird way. 🤔
December 29Teresa Marzo Lostalé