When someone is managing bipolar disorder, finding the right mood stabilizer is only half the battle. The real challenge often comes from what happens when those medications meet others in the body. Lithium, valproate, and carbamazepine are the oldest and most widely used mood stabilizers, but they don’t play well with everything. Even common over-the-counter drugs can push their levels into dangerous territory. Understanding how they interact isn’t just academic-it can mean the difference between stability and hospitalization.
Why These Three Matter
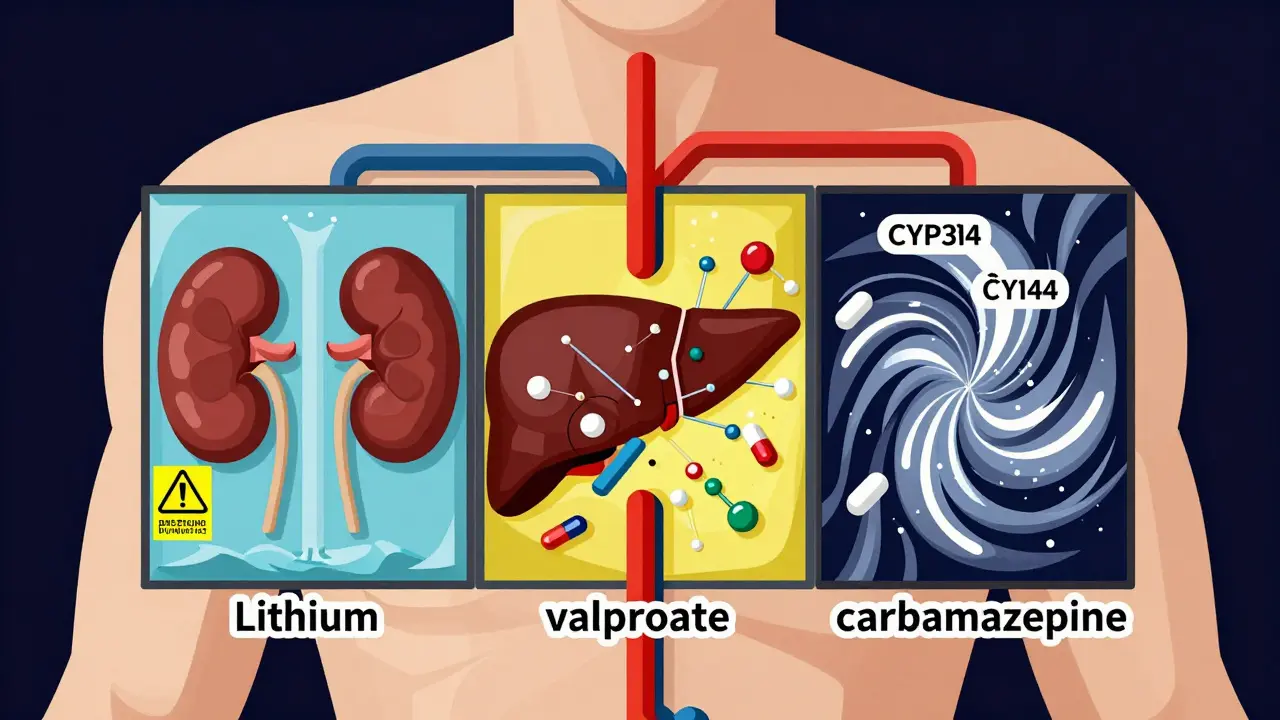
Lithium, valproate, and carbamazepine have been around for decades, but they’re still first-line treatments for bipolar disorder. Lithium was discovered in the late 1940s by Australian psychiatrist John Cade and became the first FDA-approved mood stabilizer in 1970. Valproate, originally developed as an antiseizure drug, was later found to calm manic episodes. Carbamazepine, synthesized in the 1950s, works differently from the others and is often used when lithium doesn’t work. Each has its own way of being processed by the body-and that’s where things get risky.Lithium doesn’t bind to proteins in the blood. It’s filtered out by the kidneys and nothing else. That makes it simple in theory but fragile in practice. Valproate binds tightly to proteins, gets broken down in the liver through multiple pathways, and can change how other drugs are metabolized. Carbamazepine is even trickier-it doesn’t just get broken down by the liver, it forces the liver to speed up its own breakdown over time, and it also pushes other drugs out of the system faster. These differences aren’t just textbook facts. They directly affect what happens when you take more than one medication.
Lithium: The Kidney-Dependent Risk
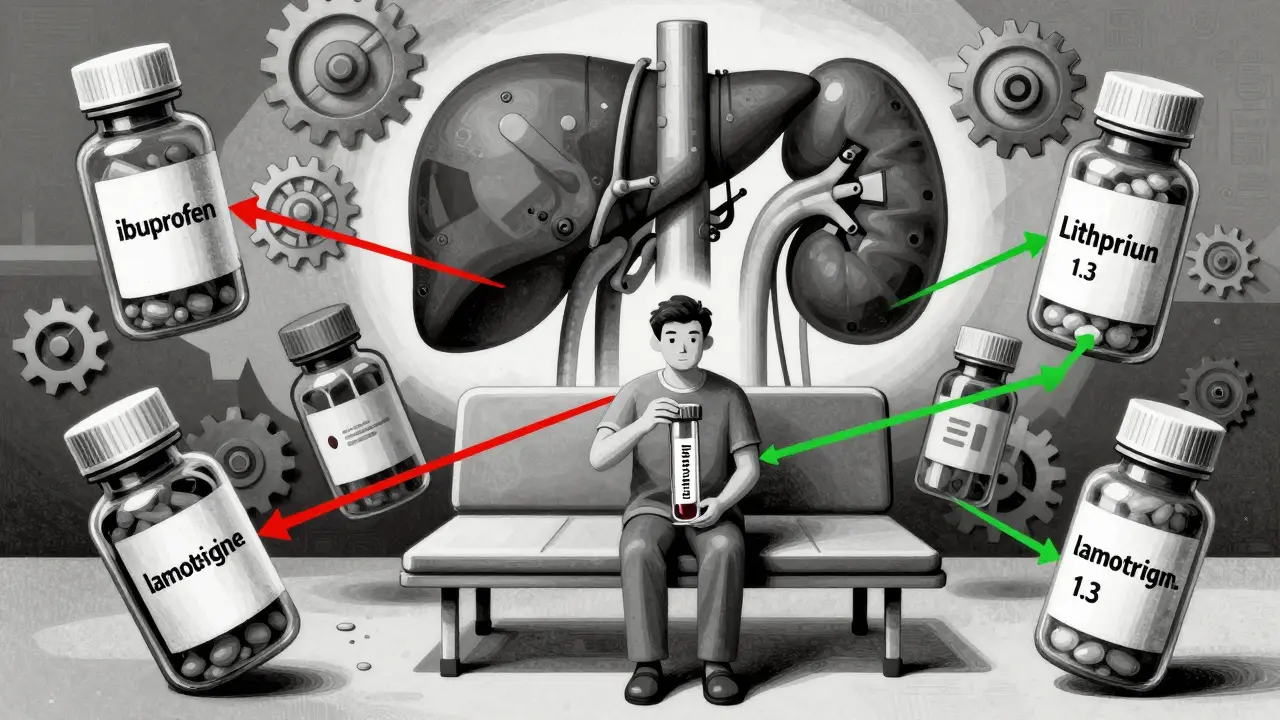
Lithium’s narrow therapeutic window-0.6 to 1.2 mmol/L-is one of the tightest in all of medicine. A small increase can cause tremors, confusion, nausea, and even seizures. The biggest danger? Medications that affect kidney function.NSAIDs like ibuprofen or naproxen are the most common offenders. A 1989 study showed that even short-term use of NSAIDs can raise lithium levels by 25-30%. That might not sound like much, but for someone stable at 0.8 mmol/L, that jump can push them into the toxic range (1.2+ mmol/L). One patient on the NAMI forum described going from mild symptoms to confusion and tremors after starting ibuprofen for a headache. Their lithium level shot up from 0.8 to 1.3 in three days.
Diuretics, especially thiazides, are another major risk. They reduce sodium in the body, which causes the kidneys to hold onto more lithium. Studies from the 1980s found thiazide diuretics can increase lithium levels by 25-40%. ACE inhibitors, often used for high blood pressure, have a similar effect. The 2020 International Society for Bipolar Disorders guidelines now recommend lowering lithium targets to 0.6-0.8 mmol/L if you’re taking any of these drugs-and checking levels within 5-7 days of starting them.
What’s surprising is what doesn’t interact with lithium. Unlike the others, it’s not affected by liver enzymes. So, antibiotics, antifungals, or even many antidepressants won’t touch it. But if you’re on anything that changes how your kidneys handle sodium or fluid, lithium is vulnerable.
Valproate: The Double-Edged Sword
Valproate is powerful, especially for acute mania. Studies show 50-60% of people respond within a week. But its interactions are complex because it does two things at once: it can block the breakdown of other drugs, and it can be broken down faster by others.One of the most dangerous combinations is valproate with lamotrigine. Valproate can double or even triple lamotrigine levels. A Reddit user shared that switching from carbamazepine to valproate forced their lamotrigine dose down from 400mg to 200mg. That’s not unusual. The 1994 Epilepsia study confirmed this effect-valproate inhibits the enzyme (UGT) that clears lamotrigine. If you’re on both, you’re at risk of a serious skin rash or even Stevens-Johnson syndrome.
On the flip side, carbamazepine can slash valproate levels by 30-50%. Why? Because carbamazepine boosts liver enzymes that break down valproate. This isn’t just theoretical. A 1997 study in Drug Metabolism and Disposition showed patients on both drugs needed higher valproate doses just to stay in range. But here’s the catch: even if valproate levels look normal, the combination can still cause neurotoxicity because carbamazepine’s active metabolite builds up.
Valproate also displaces other protein-bound drugs. That means if you’re on warfarin, phenytoin, or even some antidepressants, your free (active) levels of those drugs can spike. That’s why doctors often check levels of other medications when adding valproate-even if they’re not supposed to interact.
Carbamazepine: The Enzyme Storm
Carbamazepine doesn’t just interact-it starts a chemical war in the liver. It’s metabolized by CYP3A4, and it induces that same enzyme. That means over time, your body gets better at clearing it. That’s why your dose often needs to be increased after the first few weeks. But it doesn’t stop there. It also clears out other drugs that rely on CYP3A4.Oral contraceptives? Their effectiveness drops by 50-70%. That’s not a myth-it’s documented in the 2001 Journal of Clinical Psychopharmacology. Same goes for risperidone and haloperidol. A patient might be stable on 4mg of risperidone, then start carbamazepine and suddenly relapse because the drug is being flushed out.
But the most complex interaction is with valproate. For years, doctors thought valproate blocked the enzyme that breaks down carbamazepine’s toxic metabolite (CBZ-E). But research from 1997 showed it’s more than that. Valproate also blocks the next step-the conversion of CBZ-E into a harmless compound. That means CBZ-E builds up, even if carbamazepine levels look fine. The result? Dizziness, loss of coordination, nausea. The British Association for Psychopharmacology recommends checking both carbamazepine and CBZ-E levels when combining them, and reducing the carbamazepine dose by 25% right away.
Real-World Consequences
These aren’t abstract risks. In a 2019 survey of 853 clinicians, 74% said carbamazepine-valproate interactions were “moderately to severely problematic.” The 2021 International Bipolar Foundation survey of 1,247 patients found that 68% of lithium users needed dose changes when taking diuretics, and 22% had symptoms of toxicity.But there are success stories too. A 2022 case study in the Journal of Affective Disorders followed a patient with 12 failed medication trials. After combining lithium and valproate, they stayed stable for 18 months with no toxicity. Why? Careful monitoring. Their lithium level was kept at 0.8 mmol/L and valproate at 95 mcg/mL-both in safe, effective ranges.
The problem isn’t that these drugs don’t work. It’s that they’re not interchangeable. A patient might do great on lithium, then switch to valproate because of side effects, only to have their lamotrigine levels double and end up in the ER. Or someone might start ibuprofen for arthritis and spiral into lithium toxicity without realizing why.

What You Need to Do
If you’re on one of these drugs, here’s what matters:- For lithium: Avoid NSAIDs. If you need pain relief, use acetaminophen instead. Tell your doctor if you start any blood pressure meds, diuretics, or heart medications. Get your lithium level checked 5-7 days after any new drug is added.
- For valproate: Never combine it with lamotrigine without a dose reduction. If you’re on carbamazepine, your valproate level may drop-ask your doctor to check it. Watch for signs of liver stress: fatigue, dark urine, yellowing skin.
- For carbamazepine: Birth control won’t work. Use a backup method. Antidepressants, antifungals, and some cholesterol meds may stop working. If you add valproate, your dose of carbamazepine may need to be cut by 25%. Monitor for dizziness or unsteadiness.
There’s no universal rule. Each person’s metabolism is different. That’s why therapeutic drug monitoring-blood tests-is still the gold standard. Even with all the advances in genetics and precision medicine, nothing replaces knowing your actual drug levels.
What’s Changing Now
The landscape is shifting. Lithium prescriptions have dropped from 35% of new starts in 2012 to just 15% in 2022. Valproate’s use has fallen too-partly because of its risk to unborn babies. The FDA’s 2013 warning about birth defects cut its use in women of childbearing age by 65%. Carbamazepine use has stayed steady, but its reputation is slipping because of its interaction profile.New formulations are helping. Lithium citrate extended-release reduces peaks and valleys in blood levels. Valproate microbeads (Depakote Sprinkle) offer more stable absorption. And in the next few years, genetic testing for CYP3A4 variants may become routine before starting carbamazepine. The NIH is even running a trial (NCT05123456) to find urinary biomarkers that predict who’s at risk for lithium interactions.
But until then, the old rules still hold: know your drugs, know your levels, and never assume a new medication is safe just because it’s common.
Can I take ibuprofen with lithium?
No, not without medical supervision. Ibuprofen and other NSAIDs can raise lithium levels by 25-30%, increasing the risk of toxicity. Symptoms include tremors, confusion, nausea, and even seizures. If you need pain relief, use acetaminophen (Tylenol) instead. If you must take an NSAID, your doctor should check your lithium level within 5-7 days and may lower your lithium dose.
Why does valproate make lamotrigine levels go up?
Valproate blocks the liver enzyme UGT1A4, which is responsible for breaking down lamotrigine. This causes lamotrigine to build up in the blood-sometimes doubling or tripling its levels. This increases the risk of a dangerous skin rash like Stevens-Johnson syndrome. If you’re taking both, your lamotrigine dose will almost always need to be cut in half. Never adjust this yourself-your doctor must monitor levels closely.
Does carbamazepine affect birth control?
Yes, dramatically. Carbamazepine boosts liver enzymes that break down estrogen and progesterone. This can reduce the effectiveness of oral contraceptives by 50-70%. Even if you take them perfectly, you could still get pregnant. The CDC and FDA recommend using a backup method like condoms or an IUD while on carbamazepine. Hormonal IUDs and non-hormonal options (like copper IUD) are safer choices.
Can lithium and valproate be taken together safely?
Yes, and they’re often used together for treatment-resistant bipolar disorder. Unlike many combinations, lithium and valproate don’t directly interfere with each other’s metabolism. Lithium is cleared by the kidneys; valproate is cleared by the liver. The main concern is overlapping side effects-tremors, weight gain, or kidney stress. Doctors usually keep lithium levels low (0.6-0.8 mmol/L) and monitor kidney function closely. A 2022 case study showed this combo can work well for over a year with no toxicity if levels are carefully managed.
What’s the safest mood stabilizer for someone on other medications?
There’s no single safest option-it depends on what else you’re taking. If you’re on many other drugs, lithium may be the safest because it doesn’t interact with liver enzymes. But if you have kidney issues, it’s risky. Valproate avoids liver enzyme induction but can interfere with other drugs’ metabolism. Lamotrigine has fewer interactions overall and is often preferred when multiple medications are involved. Always discuss your full medication list with your psychiatrist. The goal isn’t the “safest” drug-it’s the one with the fewest conflicts for you.





Man, I never realized how fragile lithium is until I saw that NSAID warning. My buddy went from chill to confused in 3 days after popping ibuprofen for his back. Scary stuff. Acetaminophen it is from now on. No more 'quick fix' painkillers when you're on this stuff.
February 15Mike Hammer