Pharmacist Substitution Rules: What You Can and Can’t Swap at the Pharmacy
When you pick up a prescription, the pharmacist might hand you a different pill than what the doctor wrote on the paper. That’s not a mistake—it’s pharmacist substitution rules, the legal and clinical guidelines that let pharmacists swap brand-name drugs for generic versions when allowed. Also known as generic drug substitution, this practice keeps costs down without sacrificing safety, as long as it follows state and federal standards. These rules exist because generics are just as effective as brand names, proven through bioequivalence testing, the science that shows generic drugs absorb into the body the same way as their brand-name counterparts. The FDA requires this testing before a generic can be approved, so when your pharmacist switches your Lipitor to atorvastatin, they’re relying on solid evidence, not guesswork.
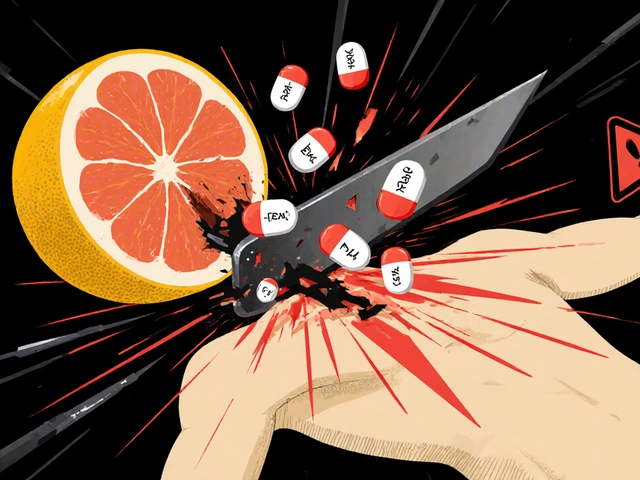
But not every drug can be swapped. prescription switching, the act of replacing one medication with another at the pharmacy is blocked in some cases—like when the drug has a narrow therapeutic index, meaning tiny changes in dose can cause big problems. Think blood thinners like warfarin, thyroid meds like levothyroxine, or seizure drugs like phenytoin. In these cases, doctors often write "Do Not Substitute" on the script, and pharmacists must follow it. Even if the generic is technically bioequivalent, the risk of subtle differences is too high. Some states also require pharmacists to notify you before swapping, or let you refuse the switch outright. You have rights here: ask why a substitution is being made, and if you’re unsure, speak up.
Then there’s the gray area: drugs that aren’t technically interchangeable but get swapped anyway. Some pharmacies push generics to cut costs, even when the difference isn’t well studied. That’s where generic medications, lower-cost versions of brand-name drugs that meet the same quality and safety standards get a bad rap—not because they’re unsafe, but because people don’t understand the rules around them. If you’ve had a bad reaction after a switch, it’s not always the generic’s fault. Sometimes it’s a change in fillers, or your body reacting to a new formulation. That’s why tracking your symptoms after a switch matters. And if you’re on multiple meds, like diabetes drugs or antidepressants, even small changes can ripple through your system. That’s why posts here cover everything from how bioequivalence testing works to why some people report different side effects with generics, and how to spot if a switch is right for you.
What you’ll find below are real, practical guides from people who’ve been there—whether it’s learning how to check if your generic is truly equivalent, understanding when to push back on a substitution, or figuring out why your pill looks different this month. You’ll see how pharmacist substitution rules play out in everyday life, from managing COPD inhalers to switching antidepressants. No jargon. No fluff. Just what you need to know to stay in control of your meds and your health.