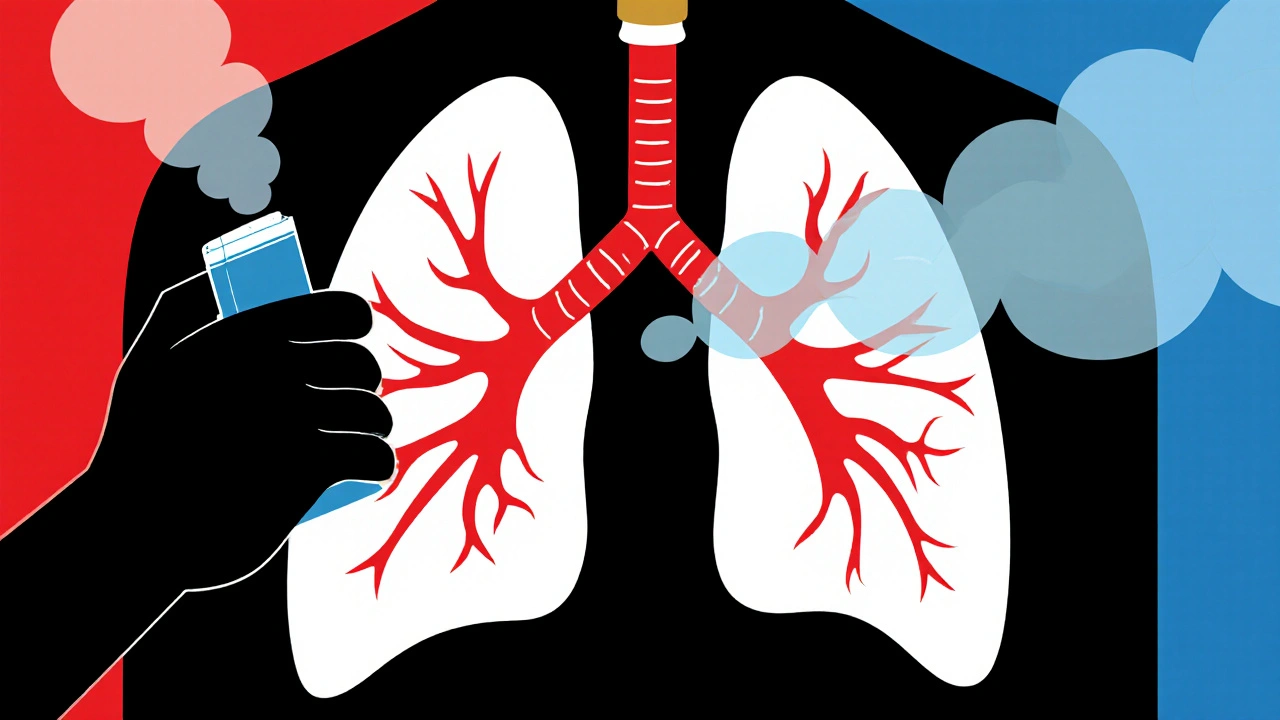
When it comes to keeping chronic obstructive pulmonary disease (COPD) stable, few medicines have the staying power of Tiotropium bromide a long‑acting muscarinic antagonist (LAMA) inhaled once daily to relax airway muscles and improve airflow. This article walks you through why it’s a cornerstone of maintenance therapy, how to use it right, and what pitfalls to watch out for.
What makes Tiotropium bromide different?
Tiotropium belongs to the LAMA class, which means it blocks the M3 receptors in the airway smooth muscle for up to 24 hours. Unlike short‑acting bronchodilators that need multiple doses a day, a single puff does the job, helping patients stick to their regimen. In the 2024 GOLD (Global Initiative for Chronic Obstructive Lung Disease) report, Tiotropium ranks at the top of preferred long‑term therapies for moderate to severe COPD because it consistently reduces exacerbations and improves health‑related quality of life.
How Tiotropium fits into the GOLD treatment ladder
The GOLD guidelines organise therapy into four groups (A‑D) based on symptom burden and risk of exacerbations. For groups B, C, and D, the recommendation is a LAMA either alone or combined with a long‑acting β2‑agonist (LABA) and/or inhaled corticosteroid (ICS). Tiotropium is the go‑to LAMA because:
- It has a well‑established safety profile from over a decade of real‑world use.
- It reduces the annual rate of moderate‑to‑severe exacerbations by 15‑20 % compared with placebo.
- It improves forced expiratory volume in one second (FEV1) by an average of 100‑150 mL, a clinically meaningful gain.
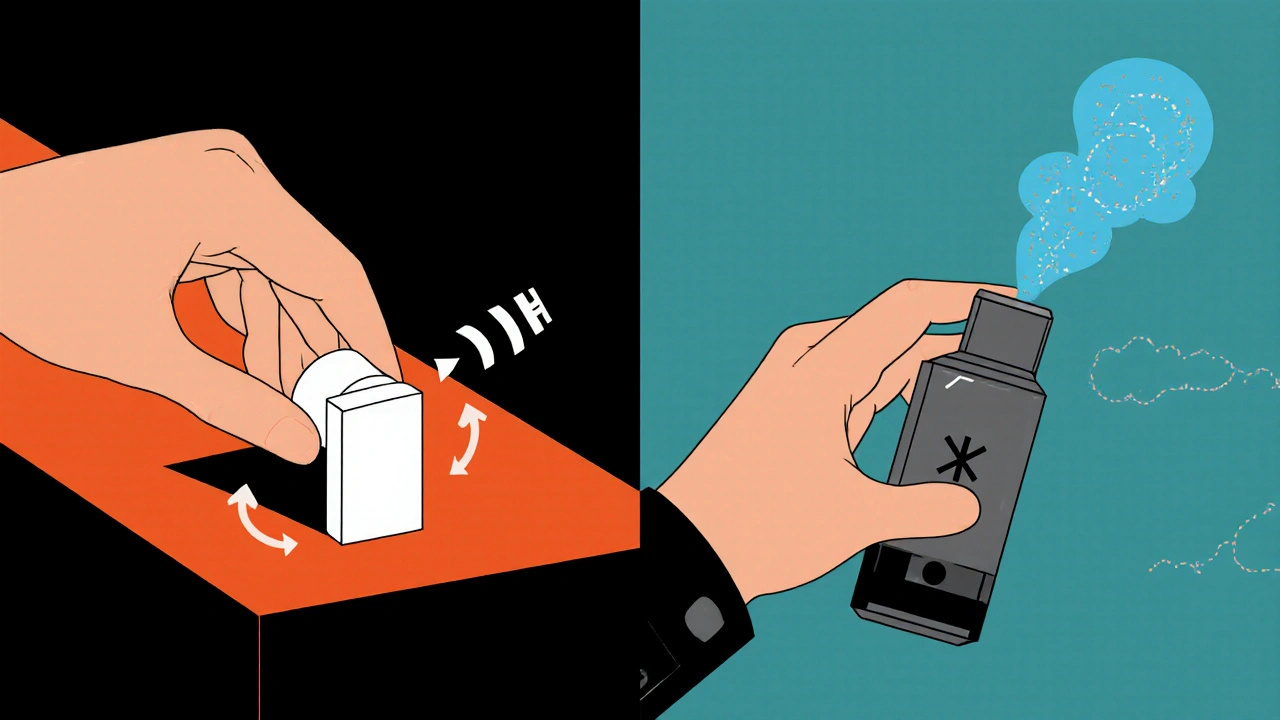
Choosing the right inhaler device
Tiotropium is marketed in two devices:
- HandiHaler - a dry‑powder inhaler (DPI) that requires the patient to load a capsule before each dose.
- Respimat - a soft‑mist inhaler that delivers the drug as a fine spray, often easier for patients with limited hand strength.
Studies show the Respimat device may achieve slightly higher lung deposition, but adherence rates are comparable when patients are trained properly.
Starting dose, administration, and titration
Regardless of device, the standard adult dose is 18 µg once daily. Here’s a quick step‑by‑step for each device:
- HandiHaler
- Insert a new capsule into the mouthpiece.
- Close the inhaler, inhale deeply through the mouth.
- Hold breath for about 10 seconds, then exhale slowly.
- Discard the used capsule.
- Respimat
- Turn the base until you hear a click - that indicates the dose is primed.
- Exhale fully, then place the mouthpiece between your lips.
- Press the dose‑release button while inhaling slowly and deeply.
- Hold breath for 10 seconds, then exhale.
There’s no need for titration; the dose is fixed. However, if a patient experiences dry mouth or cough, switching devices or adding a short‑acting bronchodilator for symptom relief can help.
Side effects, contraindications, and drug interactions
Common adverse events (AEs) include dry mouth (up to 30 % of users), throat irritation, and occasional constipation. Serious AEs such as urinary retention or narrow‑angle glaucoma are rare but worth monitoring, especially in older males.
Contraindications:
- Known hypersensitivity to tiotropium or any excipients.
- Severe renal impairment (creatinine clearance <30 mL/min) - dose adjustment may be required.
Key interactions:
- Concurrent use with anticholinergic medications (e.g., ipratropium) does not increase adverse effects but provides little added benefit.
- Beta‑blockers can blunt the effect of any LABA added to the regimen, but they do not affect tiotropium’s action.
Comparing Tiotropium with other LAMAs
| Attribute | Tiotropium (HandiHaler/Respimat) | Umeclidinium | Aclidinium |
|---|---|---|---|
| Frequency | once daily | once daily | twice daily |
| Device | HandiHaler (DPI) / Respimat (soft‑mist) | Ellipta DPI | HandiHaler DPI |
| Typical FEV1 gain | 100-150 mL | 120-160 mL | 90-130 mL |
| Exacerbation reduction | ≈15 % | ≈12 % | ≈10 % |
| Side‑effect profile | Dry mouth, cough | Similar, less cough | More throat irritation |
All three agents belong to the same pharmacologic class, so the choice often hinges on patient preference, inhaler technique, and cost considerations.
Real‑world adherence tips
Even the best drug fails if the patient forgets to use it. Here are practical strategies that have helped clinics improve adherence rates from the typical 55 % up to 80 %:
- Link the dose to a daily habit - e.g., take it right after brushing teeth in the morning.
- Use reminder apps - many inhaler manufacturers offer free smartphone alerts.
- Conduct technique checks at every visit - a quick 1‑minute demonstration catches most errors.
- Involve caregivers - for elderly patients, a family member can supervise the dose.
Tracking refill data in pharmacy software can also flag missed doses early, prompting a timely follow‑up.
When to consider combination therapy
If symptoms persist despite optimal LAMA use, the GOLD algorithm suggests adding a LABA (e.g., salmeterol, indacaterol) or an inhaled corticosteroid (ICS) for patients with frequent exacerbations or eosinophilic inflammation. The triple combo of tiotropium + a LABA + ICS (often delivered via a single inhaler) has shown further reduction in hospitalizations, but it also raises the risk of pneumonia, especially in older patients.
Future directions and emerging data
Research in 2025 is exploring ultra‑long‑acting LAMAs that could be dosed every 48 hours, potentially improving adherence even more. Meanwhile, real‑world registries continue to confirm tiotropium’s superiority in lowering mortality when compared with short‑acting bronchodilators alone.
Quick reference checklist
- Indication: maintenance therapy for COPD (moderate‑to‑severe)
- Dose: 18 µg once daily (HandiHaler capsule or Respimat spray)
- Key benefits: ↓ exacerbations, ↑ FEV1, once‑daily dosing
- Common AEs: dry mouth, throat irritation
- Contraindications: hypersensitivity, severe renal impairment
- Device choice: HandiHaler for patients comfortable with capsules; Respimat for easier inspiratory flow
- When to add LABA/ICS: persistent symptoms or ≥2 exacerbations/year
How long does Tiotropium take to start working?
Patients usually notice a smoother breathing pattern within 30 minutes, but the full bronchodilating effect builds over the first few days as the drug reaches steady‑state in the lungs.
Can I use Tiotropium together with a rescue inhaler?
Yes. Short‑acting bronchodilators like albuterol are recommended for acute symptom relief and can be taken anytime, even if you have just used your tiotropium dose.
Is Tiotropium safe for patients with asthma‑COPD overlap?
It is generally safe and is often part of the regimen for asthma‑COPD overlap, but clinicians usually add an inhaled corticosteroid to address the inflammatory component of asthma.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and resume the regular schedule - don’t double‑dose.
Are there any foods or drinks I should avoid?
No specific dietary restrictions exist, but staying well‑hydrated can lessen dry‑mouth symptoms.
How often should I see my doctor for follow‑up?
Initially, schedule a review after 4-6 weeks to confirm technique and response. After stabilization, a 6‑month routine check is typical unless you experience worsening symptoms.




In the grand theater of inhalers, the HandiHaller insists upon a ceremonial capsule‑loading ritual that borders on the absurd, as if the mere act of loading were a rite of passage for the discerning patient. One cannot help but marvel at the elegance of a device that demands a capsule for each dose, thereby guaranteeing that patients will spend precious minutes contemplating the futility of modern pharmacology. The Respimat, by contrast, offers a soft‑mist experience that pretends to be more user‑friendly, yet both devices proudly parade the same 18 µg of Tiotropium, masquerading as innovators. It is a comforting thought that a single puff can allegedly replace a lifetime of effort, isn’t it? :)
October 24Tamara Tioran-Harrison