Serotonin Syndrome Risk Checker
Risk Assessment Tool
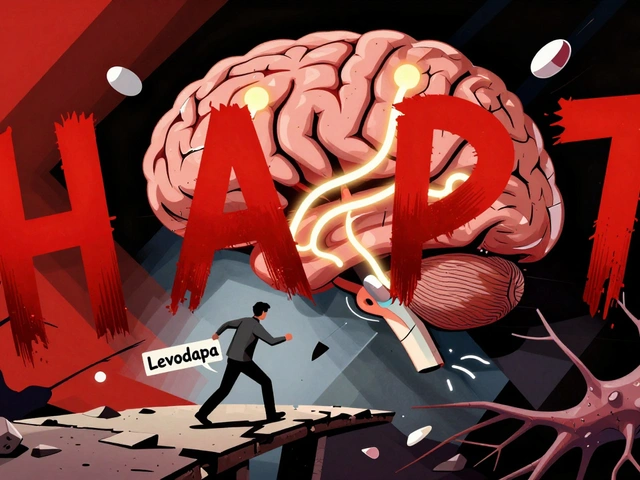
Most people think of opioids like morphine or oxycodone as painkillers that slow you down - drowsiness, constipation, maybe respiratory depression if you take too much. But tramadol isn’t like the others. It doesn’t just bind to opioid receptors. It also messes with serotonin in your brain. And that’s where things get dangerous.
Why Tramadol Is Different
Tramadol was designed to be a milder opioid, but it’s not. It works in two ways: it binds weakly to opioid receptors, and it blocks the reuptake of serotonin and norepinephrine. That second part is what makes it risky. Other opioids? They barely touch serotonin. Tramadol? It’s practically an SNRI - the same class of drugs used to treat depression. This dual action means tramadol can cause serotonin syndrome even when taken alone. That’s unheard of with drugs like hydrocodone or codeine. In fact, studies show tramadol alone has caused serotonin syndrome in people taking nothing else but the prescribed dose. One case involved a 42-year-old woman who took two 50 mg tablets and ended up with high fever, muscle rigidity, and confusion. She didn’t mix it with anything. Just tramadol.How Serotonin Syndrome Happens
Serotonin syndrome isn’t just “feeling a bit off.” It’s a medical emergency. Your body gets flooded with too much serotonin, and your nervous system goes into overdrive. Symptoms can show up in hours - sometimes within minutes after a dose. Classic signs include:- Clonus (involuntary muscle spasms, especially in the ankles)
- Hyperreflexia (overactive reflexes)
- High body temperature (over 38°C or 100.4°F)
- Sweating, shivering, or flushing
- Agitation, confusion, or hallucinations
- Rapid heart rate and high blood pressure
The Bigger Risk: Mixing with Antidepressants
The real danger comes when tramadol is taken with antidepressants - especially SSRIs like sertraline, fluoxetine, or escitalopram. This isn’t a rare accident. It’s predictable. A 2015 study of over 187,000 Medicare patients found that people taking both tramadol and an SSRI had a 3.6 times higher risk of serotonin syndrome than those on SSRIs alone. That’s not a small bump. That’s a red flag. Why? Because SSRIs block the CYP2D6 enzyme - the same enzyme your liver uses to break down tramadol. So when you take them together, tramadol builds up in your system faster than it should. You’re essentially overdosing on the serotonergic part of the drug, even if you’re taking your normal dose. Even worse, some antidepressants like fluoxetine stick around in your body for weeks. So if you stop your SSRI and start tramadol a few days later, you’re still at risk. The interaction doesn’t go away just because you stopped one drug.
Who’s Most at Risk?
Not everyone reacts the same way. Genetics play a huge role. About 7% of white people are “poor metabolizers” of tramadol because of a genetic variation in CYP2D6. That means their bodies can’t convert tramadol into its active opioid form properly - so the unmetabolized drug, which is the serotonin-blocking part, piles up. Older adults are also at higher risk. The American Geriatrics Society lists tramadol as potentially inappropriate for people over 65. Why? Because their livers and kidneys don’t clear drugs as well, and they’re more likely to be on multiple medications that interact. People with depression, bipolar disorder, or anxiety are especially vulnerable. One documented case involved a woman with bipolar II who developed serotonin syndrome and hypomania just two days after starting tramadol for fibromyalgia. She wasn’t on an antidepressant - just the painkiller. But her brain was already primed for serotonin imbalance.Real Cases, Real Consequences
A 35-year-old man in 2013 took 600 mg of tramadol with fluoxetine. He ended up in the ICU with a body temperature of 41.2°C (106.2°F), blood pressure of 210/110, and a heart rate of 142. He stayed hospitalized for three days. Another case: a 63-year-old woman on 100 mg of tramadol twice daily - exactly the prescribed dose - developed serotonin syndrome with no other drugs involved. Her symptoms cleared up after stopping tramadol. Reddit threads from pain management communities are full of similar stories. One user wrote: “I didn’t realize my 50 mg tramadol was interacting with my Lexapro until I ended up in the ER with a 104°F fever.” These aren’t outliers. They’re warnings.What Doctors Should Do
The American Society of Health-System Pharmacists recommends checking CYP2D6 status before prescribing tramadol - especially if the patient is of European descent. If they’re a poor metabolizer, switch to something else. Screen for all serotonergic drugs: SSRIs, SNRIs, MAOIs, triptans (for migraines), certain antibiotics like linezolid, even some herbal supplements like St. John’s wort. The list is longer than most people realize. If serotonin syndrome is suspected, stop tramadol immediately. Give cyproheptadine - an antihistamine that blocks serotonin receptors - and benzodiazepines to calm the nervous system. Time matters. If treated within six hours, mortality drops from 22% to under 1%.
Alternatives Exist
Tapentadol is an opioid that works like tramadol but doesn’t significantly affect serotonin. Studies show it causes serotonin syndrome at a rate 63% lower than tramadol. It’s not perfect - it still has abuse potential - but for someone on an SSRI or with a history of mood disorders, it’s a much safer choice. For neuropathic pain, gabapentin or pregabalin are often better first-line options. They don’t touch serotonin at all. And for acute pain, acetaminophen or NSAIDs like ibuprofen (if safe for the patient) are preferable.The Bigger Picture
Tramadol prescriptions in the U.S. dropped from 43 million in 2018 to 39 million in 2022. Why? Because doctors are learning. The FDA’s black box warning in 2011 about seizures, and the reclassification to Schedule II in 2014, pushed more caution into prescribing. But underreporting is still a problem. A 2021 study found only 28% of tramadol-induced serotonin syndrome cases are correctly diagnosed. Symptoms get mistaken for infection, heat stroke, or opioid withdrawal. The European Medicines Agency has already flagged tramadol’s risk-benefit profile as unacceptable for patients with psychiatric conditions. Restrictions may come to the EU by 2025.What You Should Do
If you’re on tramadol:- Don’t start any new antidepressant, migraine med, or herbal supplement without telling your doctor.
- If you feel sudden muscle stiffness, high fever, confusion, or uncontrollable shaking - seek help immediately.
- Don’t assume “I’m only taking it as prescribed” means you’re safe. Tramadol can cause serotonin syndrome alone.
- Ask your pharmacist or doctor: “Is tramadol safe with everything else I’m taking?”
- Don’t prescribe tramadol to patients on SSRIs, SNRIs, or MAOIs - period.
- Consider CYP2D6 testing for high-risk patients.
- Use the Hunter Criteria to diagnose serotonin syndrome - don’t rely on vague symptoms.
- When in doubt, choose tapentadol, gabapentin, or acetaminophen instead.




Tramadol alone caused serotonin syndrome? That’s wild. I’ve been on it for years for back pain and never knew it could do that. I’ll talk to my doctor tomorrow.
February 4Meenal Khurana