What the VA Formulary Actually Means for Veterans
If you're a veteran getting prescriptions through the VA, you've probably noticed that most of your meds are generics. That’s not an accident. The VA National Formulary is a strict, nationwide list of drugs that must be available at every VA pharmacy - and it’s built on one simple rule: use the generic version unless there’s a medical reason not to. This isn’t just policy - it’s how the VA saves billions each year while keeping care consistent across the country.
The system works because it’s mandatory. Every VA clinic, hospital, and mail-order pharmacy follows the same list. No exceptions unless your doctor proves you need a brand-name drug for clinical reasons. That’s why 92% of all prescriptions filled through the VA are generics - higher than any other major U.S. payer, including Medicare Part D or private insurance.
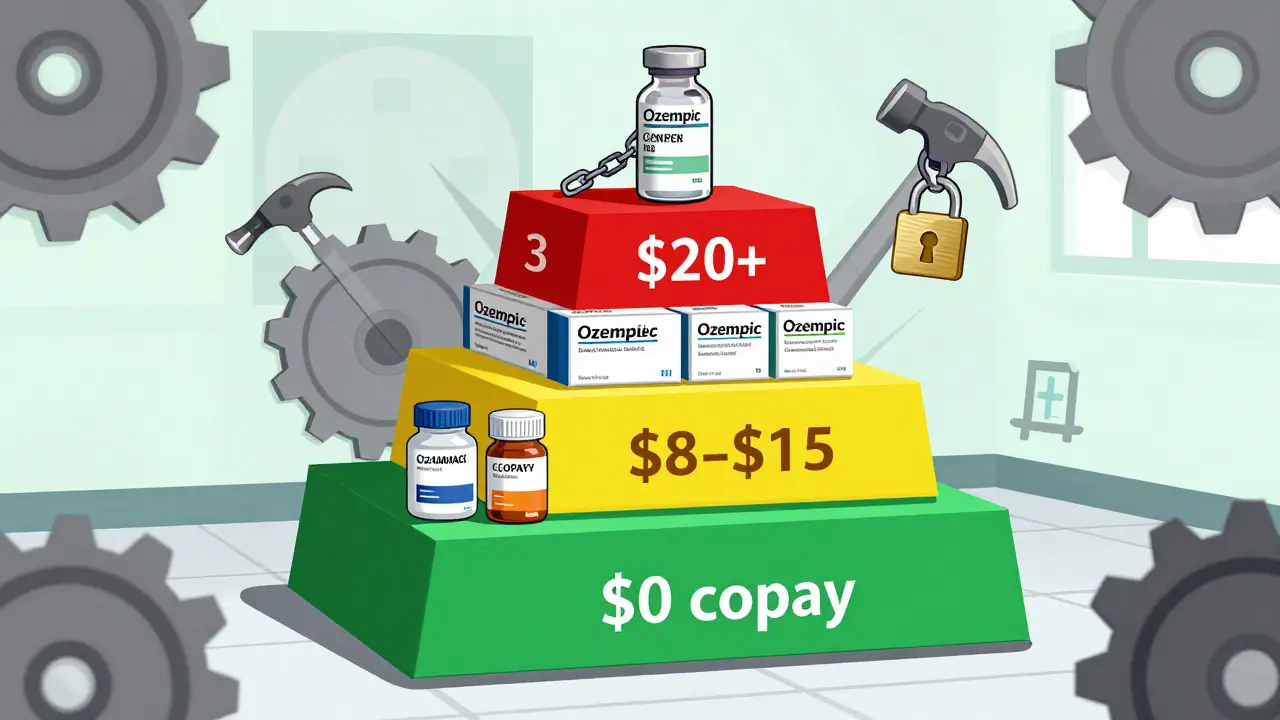
How the Three-Tier Copay System Works
Your out-of-pocket cost for a VA prescription depends on which tier the drug falls into. There are only three tiers, and it’s simple:
- Tier 1: Preferred generics. These are the cheapest. Most cost $0 to $5 for a 30-day supply. Examples: alendronate for osteoporosis, atorvastatin for cholesterol, sertraline for depression.
- Tier 2: Non-preferred generics or some brand-name drugs with generic alternatives available. Copays range from $8 to $15.
- Tier 3: Brand-name drugs with no generic available, or specialty medications. Copays can hit $20 or more.
Compare that to commercial insurance, where a Tier 5 specialty drug like Ozempic might cost $100+ per month. At the VA, if there’s a generic version - even if it’s newer - you’ll get it at Tier 1 pricing. That’s why veterans pay about $1,850 per year on average for prescriptions through the VA, while Medicare Part D beneficiaries pay over $2,300 and commercially insured patients pay nearly $2,700.
What Drugs Are Covered in 2025? Real Examples
The VA formulary is updated every month, but the big categories stay consistent. Here’s what’s covered under Tier 1 as of October 2025:
- Pain & Arthritis: Aspirin buffered tablets, ibuprofen, allopurinol
- Heart & Blood Pressure: Furosemide, hydrochlorothiazide, lisinopril
- Cholesterol: Atorvastatin, pravastatin, ezetimibe
- Mental Health: Fluoxetine, sertraline HCL, trazodone
- Diabetes: Metformin, glimepiride, insulin glargine
Notice anything? No brand names. No fancy new weight-loss drugs - unless they’re approved for diabetes. That’s because the VA’s coverage for GLP-1 medications like Wegovy or Ozempic is limited. Under CHAMPVA rules effective January 2025, these drugs are only covered for type 2 diabetes, obstructive sleep apnea, or cardiovascular risk reduction - not for weight loss alone. Veterans trying to use them for obesity may need prior authorization or pay out-of-pocket.
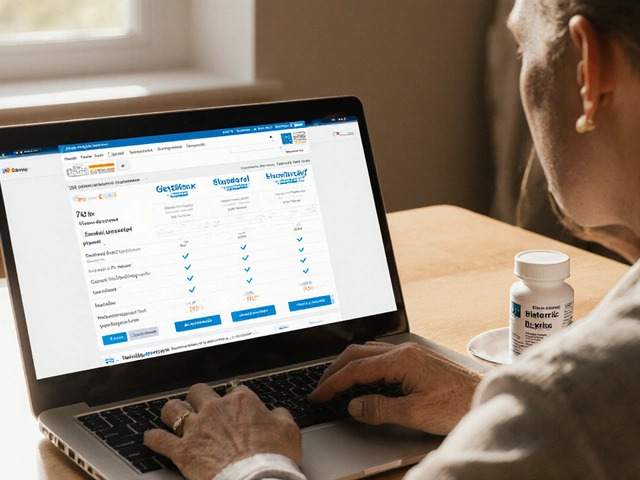
How to Check If Your Medication Is Covered
Don’t guess. Use the official VA Formulary Advisor tool. It’s free, searchable, and updated monthly. Just type in the drug name - generic or brand - and it tells you:
- Is it on the formulary?
- What tier is it?
- Is prior authorization required?
- Can it be ordered through Meds by Mail?
Many veterans don’t know this tool exists. Others assume their doctor’s prescription automatically means coverage. That’s not true. A 2024 VA survey found 35% of new enrollees were confused about tier differences - thinking a Tier 2 drug was just as cheap as Tier 1. Always check before you fill.
Meds by Mail: The Best-Kept Secret for Veterans
If you take maintenance meds - drugs you use every day - the VA’s Meds by Mail program is the easiest, cheapest way to get them. No trips to the pharmacy. No copay. No deductible. For CHAMPVA beneficiaries, it’s completely free.
You get a 90-day supply shipped directly to your home. Most Tier 1 generics arrive in 7-10 days. The system handles over 1.2 million prescriptions monthly. Veterans who use it report 87% satisfaction in VA surveys.
There are limits, though. Refrigerated biologics (like some insulin or injectable rheumatoid arthritis drugs) can’t be mailed. Some controlled substances require special handling. But for the vast majority of daily meds - blood pressure pills, antidepressants, statins - Meds by Mail is the smartest option.
Prior Authorization: When the VA Says ‘No’ - And What to Do
Not every drug is automatically approved. If your doctor prescribes a non-formulary drug - say, a newer brand-name medication with no generic - you’ll need prior authorization.
This isn’t a red tape trap. It’s a safety check. The VA’s National Drug Formulary Committee reviews each request based on clinical evidence, cost, and whether a cheaper, equally effective alternative exists. The process usually takes 3-5 business days.
Many veterans complain about delays, especially for weight-loss or rare disease drugs. One Reddit user in October 2025 wrote: “My provider wanted me on Wegovy for weight, but VA only covers it for diabetes. I had to appeal. Took 3 weeks.”
Here’s how to make it easier:
- Ask your VA provider to submit the request electronically through the e-VA system.
- Include clinical notes explaining why the generic won’t work - not just “I prefer this.”
- Call the VA Pharmacy Benefits call center at 1-800-877-8339 if you’re stuck. They handle 18,000 calls a day and can often help you track status.

Why the VA Formulary Is Different From Medicare or Private Insurance
Medicare Part D has five tiers. Private insurers have complex step therapy rules. The VA? Three tiers. No annual deductible. No pharmacy networks. No surprise bills.
And the VA doesn’t change tiers every quarter like commercial plans do. Once a drug is in Tier 1, it stays there unless a better generic comes along. That stability matters. Veterans don’t have to scramble every January when insurers restructure their formularies.
The VA’s approach is also more aggressive on generics. IQVIA says commercial payers use generics 89% of the time. The VA? 92%. That’s not just policy - it’s culture. VA pharmacists are trained to suggest generics first. Doctors are encouraged to prescribe them. It’s built into the system.
What Veterans Are Saying - And What’s Really Changing
Most veterans are happy. A September 2025 Reddit post from user ArmyVet2010 said: “Switched to generic sertraline through VA Mail Order. Same as Zoloft, costs me $0. My local pharmacy wanted $15.”
But there are frustrations. Veterans with rare diseases, cancer, or complex conditions sometimes hit walls. The VA’s formulary committee is slow to add new specialty drugs. In 2024, the VA Office of Inspector General reported a 12.3% jump in specialty drug spending - below the national average of 15.7%, but still rising.
The VA is responding. By Q3 2026, they plan to roll out AI tools in electronic health records that automatically suggest generic alternatives when a doctor prescribes a brand-name drug. It’s not about pushing meds - it’s about reducing waste and keeping costs down so the system lasts.
What You Need to Do Now
If you’re a veteran on VA benefits, here’s your action list:
- Go to VA Formulary Advisor and search every medication you take.
- Ask your provider: “Is there a generic version on the VA formulary?” If yes, request it.
- Enroll in Meds by Mail for maintenance drugs - it’s free and convenient.
- If a drug is denied, ask for the reason and whether prior authorization is possible.
- Keep a printed copy of your formulary status - especially if you use community care.
The VA doesn’t always get it right. But its formulary system is the most cost-effective, transparent, and veteran-focused pharmacy program in the country. Understanding it isn’t just helpful - it’s how you make sure you’re getting the full benefit you’ve earned.



I never realized how much I was overpaying at my local pharmacy until I switched to VA Meds by Mail. Now I get my sertraline for free and it’s the exact same as Zoloft. Honestly? I wish more people knew about this.
February 2Rachel Kipps