When you take a pill, you expect it to work-fast enough to help, but not so fast that it hurts. That’s where the difference between extended-release and immediate-release medications becomes life-changing. One keeps your drug levels steady for hours. The other hits you hard and fast. Mixing them up, or taking them wrong, can lead to serious side effects-or even overdose.
How These Two Types Work
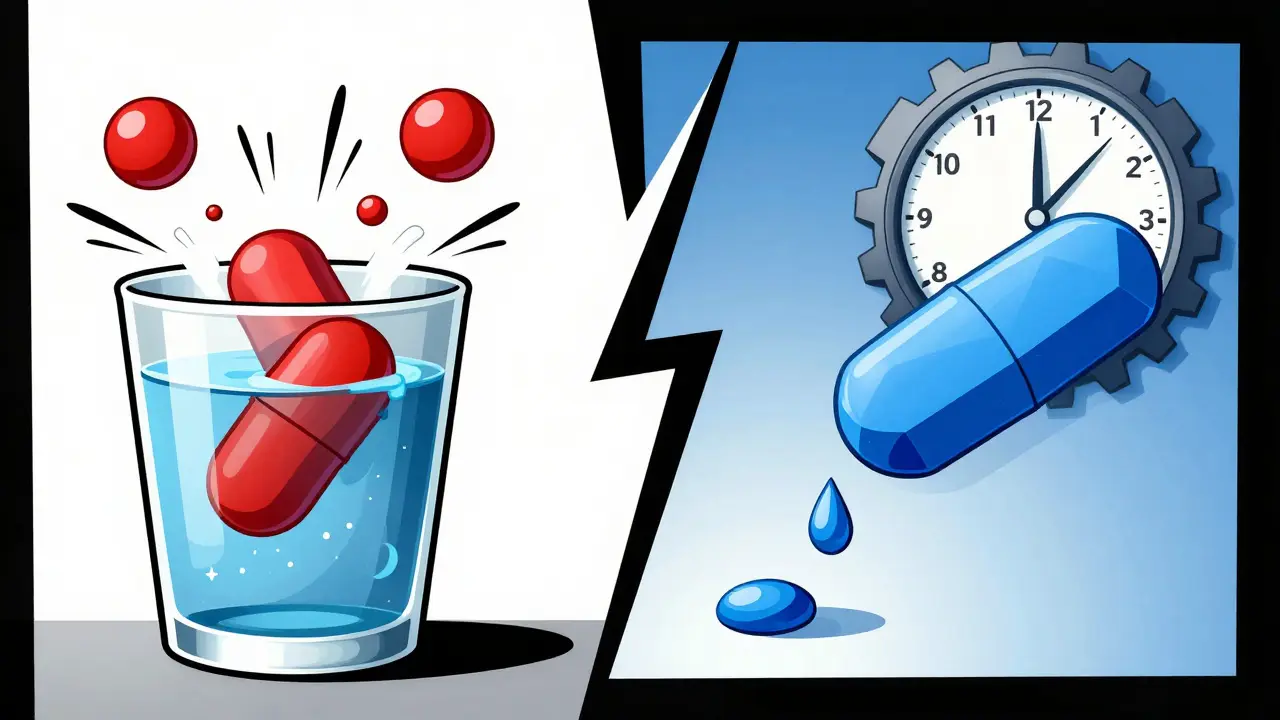
Immediate-release pills dissolve quickly in your stomach. Within 15 to 30 minutes, your body starts absorbing the full dose. Peak levels hit in under two hours, and the effect fades in 4 to 8 hours. That’s why you might need to take an IR painkiller three times a day. It’s simple, fast, and predictable. Extended-release pills, on the other hand, are built like tiny time machines. They use special coatings, gels, or tiny pellets that slowly leak out the drug over 12 to 24 hours. You take one pill, and it works all day. Brands like Concerta, Adderall XR, and Metformin ER use tech like osmotic pumps or hydrophilic matrices to control how fast the medicine flows into your bloodstream. The goal? Keep your drug levels smooth-no spikes, no crashes. Instead of peaking at 600 ng/mL and dropping to 50 ng/mL within hours (like IR bupropion), ER versions hold steady between 100-200 ng/mL all day. That’s why doctors prefer them for chronic conditions: fewer side effects, fewer doses, better adherence.When Speed Matters: Why Immediate-Release Still Has a Place
ER sounds better, right? Not always. If you’re having a panic attack, a sudden spike in pain, or a manic episode, waiting 2-4 hours for an ER pill to kick in isn’t an option. That’s where immediate-release shines. A single 5mg IR Adderall tab can snap you into focus within 30 minutes for a big meeting. An IR opioid like oxycodone can knock out breakthrough pain when your ER painkiller isn’t enough. In psychiatric care, clinicians often start patients on IR versions to find the right dose. Once stabilized, they switch to ER for long-term control. Trying to titrate a patient on ER alone? You’re playing roulette with side effects. It takes 7-10 days for ER meds to reach steady state-twice as long as IR. If you increase the dose too soon, thinking it’s not working, you risk accidental overdose.The Hidden Dangers of Extended-Release
ER meds aren’t safer just because they’re slower. They’re more dangerous if you break the rules. Ninety-two percent of extended-release tablets cannot be crushed, chewed, or split. Doing so destroys the release mechanism. A patient who crushes a 150mg Venlafaxine XR tablet? They just swallowed 150mg all at once-like an IR overdose. The FDA issued warnings about this exact risk with ER opioids in 2020. Hundreds of ER-related overdoses each year happen because someone thought, “This pill’s too big,” and broke it open. Even worse, ER overdoses last longer. If you take too much ER bupropion, the drug keeps leaking into your system for 24 to 48 hours. That means hospital stays are 2-3 times longer than with IR overdoses. The poison control system reports that ER drug poisonings are harder to treat because the body keeps getting more drug, even after you’ve been stabilized.
Who Benefits Most From Extended-Release?
If you’re on a daily medication for depression, high blood pressure, ADHD, or diabetes, ER is often the smarter choice. A 2022 JAMA study tracked 15,000 people with hypertension. Those on ER versions had a 22% higher adherence rate. Why? One pill a day beats three. No midday dosing at work. No forgetting the afternoon pill. Patients on ER metoprolol reported 32% fewer dizziness episodes-likely because their blood pressure didn’t swing wildly. For ADHD, Adderall XR gives 10-12 hours of control. IR lasts 5-8. That means no more school nurses administering pills at noon. No more awkward “I need to take my pill” moments at the office. On Reddit’s ADHD community, 68% of users said they preferred XR for daily focus, even though it takes longer to start. The CDC found that 68% of new antidepressant prescriptions in 2022 were ER. That’s not random. SSRIs like sertraline ER offer smoother mood control, fewer nighttime awakenings, and less nausea than their IR cousins.Cost, Convenience, and Confusion
ER versions usually cost 15-25% more than IR. Adderall XR runs $350-$450 for 30 capsules. Adderall IR? $280-$380. But here’s the catch: you’re not just paying for the drug. You’re paying for fewer trips to the pharmacy, fewer missed doses, and fewer ER visits from side effects. Still, confusion is common. A GoodRx survey of 5,000 chronic medication users found 41% didn’t understand why their ER pill wasn’t working right away. Some took extra doses because they felt nothing after an hour. Nine percent ended up with adverse events-nausea, dizziness, even heart palpitations-from unintentional overdosing. Pharmacists see this all the time. Twenty-three percent of ER medication errors come from people splitting pills. Venlafaxine XR isn’t scored. Crushing it? Dangerous. But patients do it anyway. “I can’t swallow big pills,” they say. That’s when you need to ask your doctor: Is there a liquid form? A smaller tablet? A different ER option?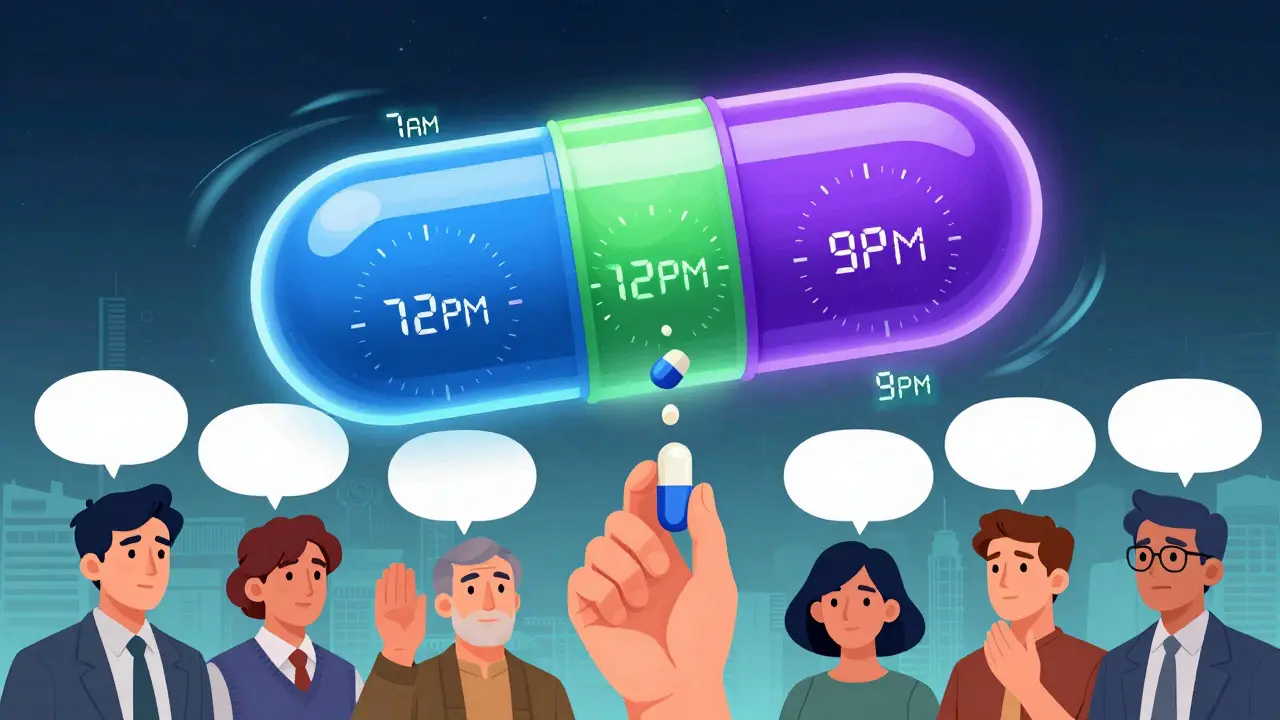
What You Need to Know Before You Take It
Here’s the practical checklist:- Never crush, split, or chew any ER pill unless the label says it’s safe. If it’s an osmotic pump (like Concerta), it’s never safe.
- Wait 7-10 days before deciding if your ER medication “isn’t working.” It takes longer to build up in your system.
- Know your timing. ER takes 2-4 hours to start. IR starts in 30 minutes. Don’t confuse delayed onset with ineffectiveness.
- Keep IR on hand if you’re on ER for chronic conditions. A small dose of IR can help with breakthrough symptoms-like sudden anxiety or pain-but only if your doctor approves it.
- Check your stomach. If you have gastroparesis (delayed stomach emptying), ER meds can absorb unpredictably. The FDA warned in 2023 that these patients can get 30-50% higher drug peaks, increasing overdose risk.
What’s Next for Medication Delivery?
The future of pills is getting smarter. New ER tech like Aversion®-used in some ADHD meds-turns crushed pills into thick gels to deter abuse. MIT researchers are testing 3D-printed “polypills” that release different drugs at exact times. Imagine one pill that gives you your blood pressure med at 7 a.m., your cholesterol drug at noon, and your sleep aid at 9 p.m. But until then, the choice between ER and IR isn’t about what’s newer. It’s about what’s right for your body, your lifestyle, and your safety. If you’re switching from IR to ER-or vice versa-talk to your pharmacist. Ask: “Is this safe to split?” “How long until it starts working?” “What happens if I miss a dose?” Don’t assume. Don’t guess. Your life depends on getting it right.Can I split an extended-release pill in half?
Only if the pill is specifically labeled as scored and safe to split. Most extended-release tablets-like Venlafaxine XR, Adderall XR, or Concerta-are not designed to be split. Crushing or splitting them can release the entire dose at once, leading to dangerous overdose. Always check the prescribing information or ask your pharmacist before splitting any pill.
Why does my extended-release medication take so long to work?
Extended-release pills are designed to release medication slowly over 12-24 hours, so they take 2-4 hours to reach therapeutic levels. This is normal. If you feel no effect after an hour, don’t take another dose. Doing so can cause accidental overdose. It can take 7-10 days for the full effect to build up in your system.
Is extended-release always better than immediate-release?
No. ER is better for long-term, stable conditions like depression, ADHD, or high blood pressure where steady levels reduce side effects. But IR is better for acute symptoms-like sudden pain, panic attacks, or when adjusting doses. Many patients use both: ER for daily control and IR for breakthrough symptoms, under doctor supervision.
What happens if I accidentally take two extended-release pills?
Call poison control immediately (1-800-222-1222 in the U.S.). ER medications release drug over hours or days, so an overdose doesn’t peak right away. You might feel fine at first, but the drug continues to enter your bloodstream. Hospital stays for ER overdoses are often 2-3 times longer than for IR because the body keeps absorbing the medication.
Can I switch from immediate-release to extended-release on my own?
Never switch without your doctor’s guidance. ER and IR versions are not always dose-for-dose equivalent. For example, 30mg of Adderall IR is not the same as 30mg of Adderall XR in how it affects your body. Your doctor will adjust the dose and timing based on your needs and how your body responds to each formulation.
Are extended-release medications more expensive?
Yes, ER versions typically cost 15-25% more than IR. For example, Adderall XR can cost $350-$450 for 30 capsules, while Adderall IR runs $280-$380. But the higher cost can be offset by fewer pharmacy visits, fewer side effects, and lower risk of hospitalization due to missed doses or overdose.



So let me get this straight - you pay $450 for a pill that you can’t even crush, chew, or look at funny, and if you do, you’re basically doing a slow-motion suicide? 🤡
January 12And the worst part? Your pharmacist looks at you like you just asked if you can microwave your thyroid.
I’ve seen people split ER pills like they’re breaking a chocolate bar. ‘It’s too big, I can’t swallow it.’ Bro, you’re not eating a Tums, you’re playing Russian roulette with your liver.
And don’t even get me started on the ‘I didn’t feel anything after an hour’ crowd. Yeah, because your body isn’t a Netflix binge - it doesn’t load in 30 seconds.
Also, why is the FDA the only one who cares that people are turning Adderall XR into a powder and snorting it? Because apparently, we’re all just one bad decision away from a 72-hour ER stay.
My grandma takes one ER pill a day and lives longer than most of us who think ‘fast-acting’ means ‘I’ll feel better before my coffee cools.’
And yet, somehow, the internet is full of people trying to ‘optimize’ their meds like they’re tuning a car engine.
Stop. Just stop.
Read the label.
Ask your pharmacist.
Don’t be the reason someone has to write a post called ‘How I Accidentally Poisoned Myself With My Own ADHD Meds.’
Windie Wilson