More than 1 in 5 people worldwide have a fungal skin infection at any given time. You might not realize it, but that itchy red patch on your groin, the flaky ring on your arm, or the persistent redness between your toes could be more than just dry skin or eczema. Fungal skin infections like Candida and ringworm are common, often misunderstood, and surprisingly easy to treat-if you know what you’re looking for.
What Exactly Is a Fungal Skin Infection?
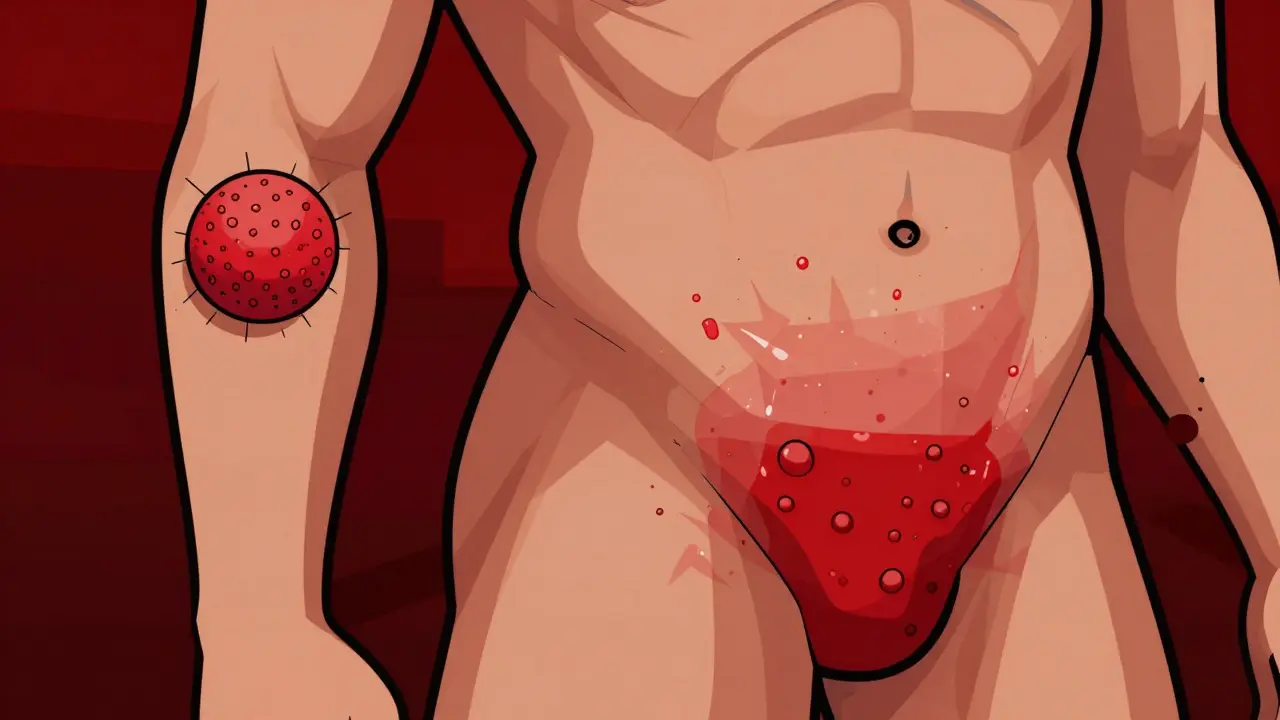
Fungal skin infections happen when microscopic fungi, which normally live harmlessly on your skin, start to overgrow. These fungi feed on keratin, a protein found in skin, hair, and nails. Two main types cause most problems: dermatophytes (which cause ringworm) and Candida (a type of yeast). Ringworm isn’t caused by worms-it’s a name from the 1800s because the infection often forms a circular, red, scaly patch with a raised edge and clearer center. Candida infections, on the other hand, don’t form rings. Instead, they show up as bright red, moist, sometimes pimple-covered rashes in warm, sweaty areas like armpits, under breasts, or in diaper areas. The difference matters because treatments vary. Using the wrong cream can delay healing or make things worse.Ringworm: The Classic Circular Rash
Ringworm, or tinea, is caused by fungi from three main groups: Trichophyton (responsible for 80-90% of cases), Microsporum, and Epidermophyton. It’s contagious and spreads easily through skin contact, shared towels, or even pets. Cats and dogs, especially puppies and kittens, are common carriers. There are different types based on where they appear:- Tinea corporis: Body rash-circular, red, scaly, with a raised border
- Tinea pedis: Athlete’s foot-between the toes, peeling, itchy, sometimes smelly
- Tinea cruris: Jock itch-in the groin, inner thighs, often worse with sweating
- Tinea unguium: Nail fungus-thick, yellow, crumbly nails
- Tinea capitis: Scalp infection-common in kids, causes patches of hair loss
Candida: The Yeast That Loves Moisture
Candida albicans is the most common culprit. It’s not contagious like ringworm-it’s already on your skin and in your gut. When conditions get warm and damp, it multiplies. That’s why diaper rashes in babies, under-breast rashes in overweight adults, and vaginal yeast infections are all forms of candidiasis. Candida rashes look different from ringworm:- Deep red, shiny, and moist
- Often have small red bumps (satellite pustules) around the edges
- Can be painful or burn, not just itch
- Common in skin folds: armpits, under breasts, between fingers, groin

Antifungals: What Works and What Doesn’t
Not all antifungal creams are the same. The two main classes are azoles and allylamines.- Azoles (clotrimazole, miconazole): Good for Candida and mild ringworm. Available over the counter. Apply twice daily for 2-4 weeks.
- Allylamines (terbinafine): Better for ringworm, especially stubborn cases. Works faster-often clears in 1-2 weeks. Also available OTC.
Why Do These Infections Keep Coming Back?
Recurrent infections are frustrating-and common. About 35% of people who’ve had ringworm or Candida get it again within a year. Why?- Incomplete treatment: People stop using the cream when the rash looks better, but the fungus is still there. That’s why you need to keep applying for the full course-even if it’s 4 weeks.
- Moisture traps: Tight clothes, sweaty gym gear, not drying skin folds after showering-all keep fungi thriving.
- Shared items: Towels, combs, shoes, gym mats. Ringworm spreads like wildfire in locker rooms.
- Underlying conditions: Diabetes, obesity, or a weakened immune system make recurrence more likely.
What About Natural Remedies and Probiotics?
You’ve probably heard about tea tree oil, coconut oil, or probiotics for fungal infections. Some people swear by them. There’s limited scientific backing for tea tree oil-it might help mild cases, but it’s not reliable enough to replace proven treatments. Coconut oil has some antifungal properties in lab studies, but real-world results are mixed. Probiotics? More promising. A 2023 survey of 850 people with recurrent vaginal Candida found that 65% had fewer flare-ups when they took Lactobacillus probiotics alongside antifungals. While not a cure, it helps restore balance. For diaper rash, adding probiotic drops to formula or applying probiotic powder to the skin (under medical guidance) has shown benefit in small studies. Don’t rely on these alone-but they can be useful sidekicks to your treatment plan.
When to See a Doctor
You don’t always need to see a doctor for a rash. But here’s when you should:- The rash doesn’t improve after 2 weeks of OTC treatment
- It spreads quickly or gets worse
- You have diabetes, HIV, or take immunosuppressants
- The rash is on your scalp, nails, or face
- You’re not sure if it’s ringworm, eczema, or psoriasis
Preventing Fungal Skin Infections
Prevention is easier than treatment:- Dry skin thoroughly after showers, especially between toes, under breasts, and in the groin
- Wear breathable cotton underwear and loose clothing
- Avoid walking barefoot in public showers or pools
- Don’t share towels, shoes, or hairbrushes
- Change out of sweaty clothes right after exercise
- Keep pets clean and check for bald patches-they might be carriers
- If you have diabetes, control your blood sugar-it’s one of the biggest risk factors