Splitting or crushing pills might seem like a simple fix-maybe you’re trying to save money, make it easier to swallow, or adjust a dose. But if you don’t do it right, you’re not just risking an inaccurate dose. You could be exposing yourself or someone else to dangerous contamination. In care homes, hospitals, and even at home, improper pill splitting has led to serious errors: one resident getting too much warfarin because a splitter wasn’t cleaned, a nurse inhaling cancer drug particles from an open crusher, or a child accidentally swallowing a crushed tablet meant for an adult. This isn’t theoretical. It’s happening right now.
Not All Pills Can Be Split or Crushed
Before you even pick up a splitter, check the pill. A lot of medications are designed to release slowly, protect the stomach, or stay stable until they reach a certain part of the gut. Crushing or splitting these can destroy that design-and turn a safe drug into a dangerous one.
Never split or crush:
- Enteric-coated pills (they have a shiny outer layer to prevent stomach irritation)
- Sustained-release or extended-release tablets (marked ER, SR, XR, LA)
- Capsules (unless the pharmacist says it’s safe to open them)
- Hazardous drugs like chemotherapy agents (cyclophosphamide, methotrexate)
- Sublingual or buccal tablets (meant to dissolve under the tongue)
According to the FDA, 97.8% of these types of pills should never be altered. If the tablet has a score line, that’s a clue-but not a guarantee. Some scored tablets still shouldn’t be split because the coating or formulation makes them unstable after splitting. Always check with your pharmacist before splitting anything.
Use the Right Tool-Not Scissors or a Knife
Using scissors, a knife, or even your fingers to split a pill is one of the most common mistakes. It’s messy, inaccurate, and dangerous. A 2021 study from the University of Jordan found that splitting with scissors resulted in 63.7% dose accuracy. That means almost two out of every three splits gave the wrong amount of medicine.
What you need is a dedicated pill splitter with a v-shaped holder and a sharp, stainless steel blade. These tools are designed to cut pills cleanly and evenly. Look for models with a retractable blade and a cover to contain dust. Brands like Med-Plus Pro and Express Scripts’ recommended models have been tested to achieve 94.7% contamination-free splits.
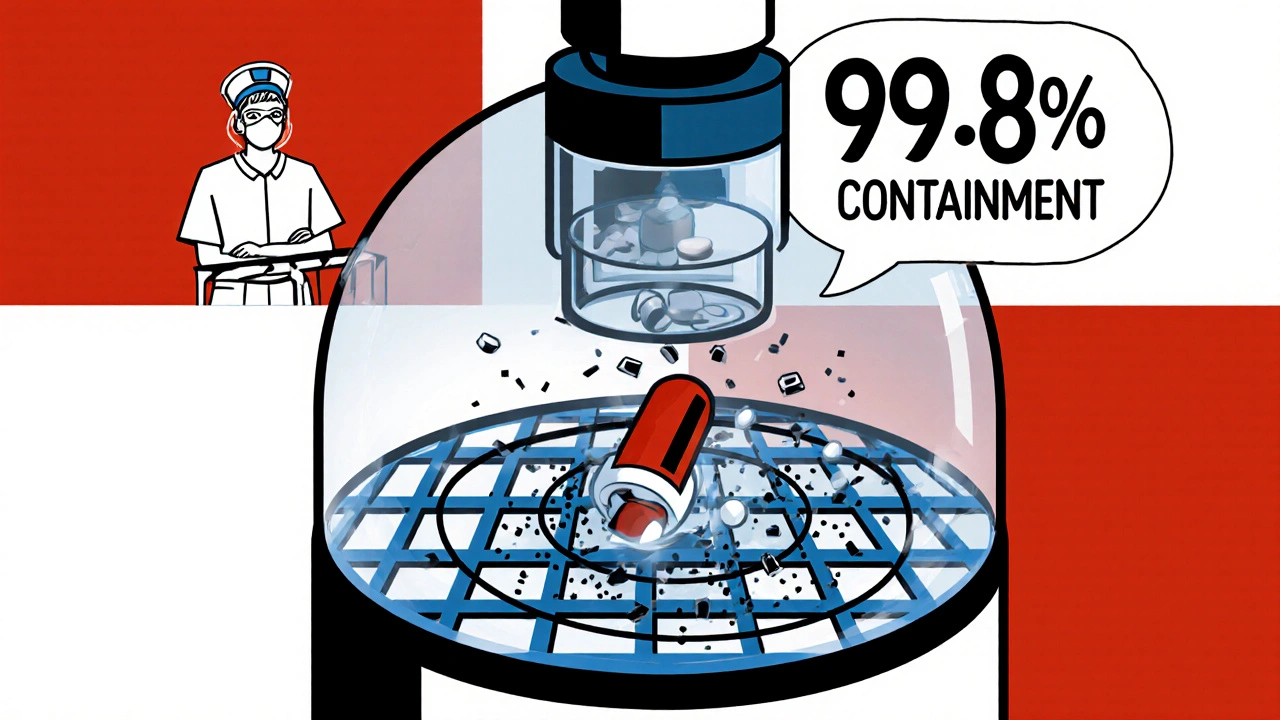
For crushing, never use a mortar and pestle or crush pills in a plastic bag. Use a closed-system pill crusher like the Silent Knight. These devices seal the pill inside a chamber during crushing, capturing over 99.8% of the powder. Open crushing can release fine particles into the air-especially dangerous with hazardous drugs. NIOSH testing shows open methods allow up to 28% of toxic dust to escape. That’s enough to settle on your skin, clothes, or countertops.
Clean Between Every Use-No Exceptions
One of the biggest causes of contamination is reusing equipment without cleaning it. Imagine splitting a blood thinner like warfarin, then using the same splitter for an antibiotic. Residue from the first pill can transfer to the second. That’s not just contamination-it’s a medical error.
Every time you switch medications, clean the splitter or crusher:
- Wipe all surfaces with a 70% isopropyl alcohol wipe.
- Let it air dry completely before the next use.
- Never share equipment between patients unless it’s been professionally sterilized.
Studies show that only 34.6% of care home staff clean their splitters between different meds, even though guidelines say they must. This is a major reason why 8.3% of medication errors in institutions come from improper splitting or crushing.
For hazardous drugs, use disposable liners or single-use crushers. Some facilities now assign a dedicated splitter to each resident to avoid cross-contamination entirely. At Sunrise Senior Living, this approach cut medication errors by 32.5% in just six months.
Don’t Split a Whole Month’s Supply at Once
It’s tempting to split all your pills for the week-or even the month-on Sunday night. Don’t.
The FDA explicitly warns against pre-splitting. Once you break a tablet, you expose the medicine to air, moisture, and light. That can make it less effective-or even unsafe. Some medications degrade within hours. Others become unstable and start to clump or change chemical structure.
Split pills right before you take them. If you need to prepare ahead, only split one day’s dose at a time and store it in a dry, cool place. Even then, use it within 24 hours. Some European guidelines allow pre-splitting with lab testing for stability-but that’s not something you can do at home.
Wash Hands and Wear Gloves
Before handling any pills, wash your hands with soap and water for at least 20 seconds. Then put on disposable gloves. This isn’t just about contamination from the pill-it’s about contamination from your skin.
Oil, sweat, and dead skin cells can transfer to the pill surface. That’s not a big deal for most medications-but with potent drugs like hormone therapies or cancer treatments, it matters. In one 2019 study, healthcare workers handling crushed cyclophosphamide without gloves had measurable levels of the drug on their skin: 4.7 ng/cm². That’s enough to cause long-term health risks with repeated exposure.
After handling, dispose of gloves properly and wash your hands again. Don’t touch your face, phone, or food until you’ve cleaned up.
Know the Risks with Hazardous Drugs
If you’re crushing or splitting chemotherapy drugs, immunosuppressants, or other hazardous medications, you’re dealing with a whole different level of risk. These aren’t just pills-they’re toxic substances.
OSHA’s updated Hazardous Drugs Standard (effective January 1, 2025) requires all healthcare facilities to use closed-system devices for crushing these drugs. No exceptions. Even a tiny amount of powder inhaled or absorbed through the skin can cause reproductive harm, organ damage, or cancer over time.
Home caregivers often don’t realize they’re handling hazardous drugs. If a loved one is on a cancer drug, ask the pharmacist: “Is this a hazardous medication?” If yes, you must use a closed-system crusher and follow strict cleanup rules. Never crush these in the kitchen or near food.

Pharmacist Involvement Reduces Errors
One of the most effective ways to prevent contamination and errors is to involve your pharmacist. They know which pills can be split, which need special equipment, and how to label them correctly.
A 2022 study in JAMA Internal Medicine found that when pharmacists educated Medicare patients on safe splitting practices, medication errors dropped by 58.3%. That’s not a small number. That’s life-changing.
Ask your pharmacist:
- “Can this pill be safely split or crushed?”
- “Do I need a special device?”
- “Should I use gloves or clean the splitter?”
- “Is there a liquid or alternative form available?”
Many pharmacies now offer pre-split pills for common medications. It’s cheaper than buying a splitter, and it eliminates the risk entirely.
What If You’ve Already Been Doing It Wrong?
If you’ve been splitting pills with scissors, crushing tablets in a cup, or reusing the same splitter for weeks-you’re not alone. But it’s time to stop.
Start by:
- Stopping all splitting or crushing until you’ve checked with your pharmacist.
- Buying a proper pill splitter or closed-system crusher.
- Throwing away any old splitters that aren’t designed for medication use.
- Labeling each splitter with the resident’s name or medication type to avoid mix-ups.
- Training anyone else who helps with meds-family members, caregivers, nurses.
Don’t wait for a mistake to happen. The cost of a wrong dose-hospitalization, overdose, poisoning-is far higher than the cost of a $15 splitter.
Final Check: Your Safety Checklist
Before you split or crush any pill, run through this quick checklist:
- ✓ Is this pill on the FDA’s list of non-splittable medications?
- ✓ Do I have a proper pill splitter or closed-system crusher?
- ✓ Have I cleaned the device with alcohol wipes since the last use?
- ✓ Am I wearing gloves?
- ✓ Am I splitting only what I need right now?
- ✓ Did I wash my hands before and after?
- ✓ Did I check with my pharmacist?
If you answered ‘no’ to any of these, don’t proceed. Stop. Call your pharmacist. Get it right.
Safety isn’t about being perfect. It’s about knowing the risks and taking simple, consistent steps to avoid them. One clean splitter, one pair of gloves, one question to your pharmacist-that’s all it takes to prevent a disaster.






Just split my mom's pills with a knife for years. Didn't even know it was dangerous. Thanks for the wake-up call.
November 14Amie Wilde