Snoring isn’t just annoying-it can wreck sleep for you and your partner, and sometimes it’s a sign of something more serious. If you’ve tried pillows, nasal strips, or sleeping on your side and still hear that loud rhythm night after night, you might be wondering if there’s a real solution. Oral appliance therapy using mandibular advancement devices (MADs) is one of the most effective, non-invasive options backed by decades of clinical research. Unlike CPAP machines, which require masks and air pressure, MADs are small, custom-fit devices worn like mouthguards that gently move your lower jaw forward to keep your airway open.
How Mandibular Advancement Stops Snoring
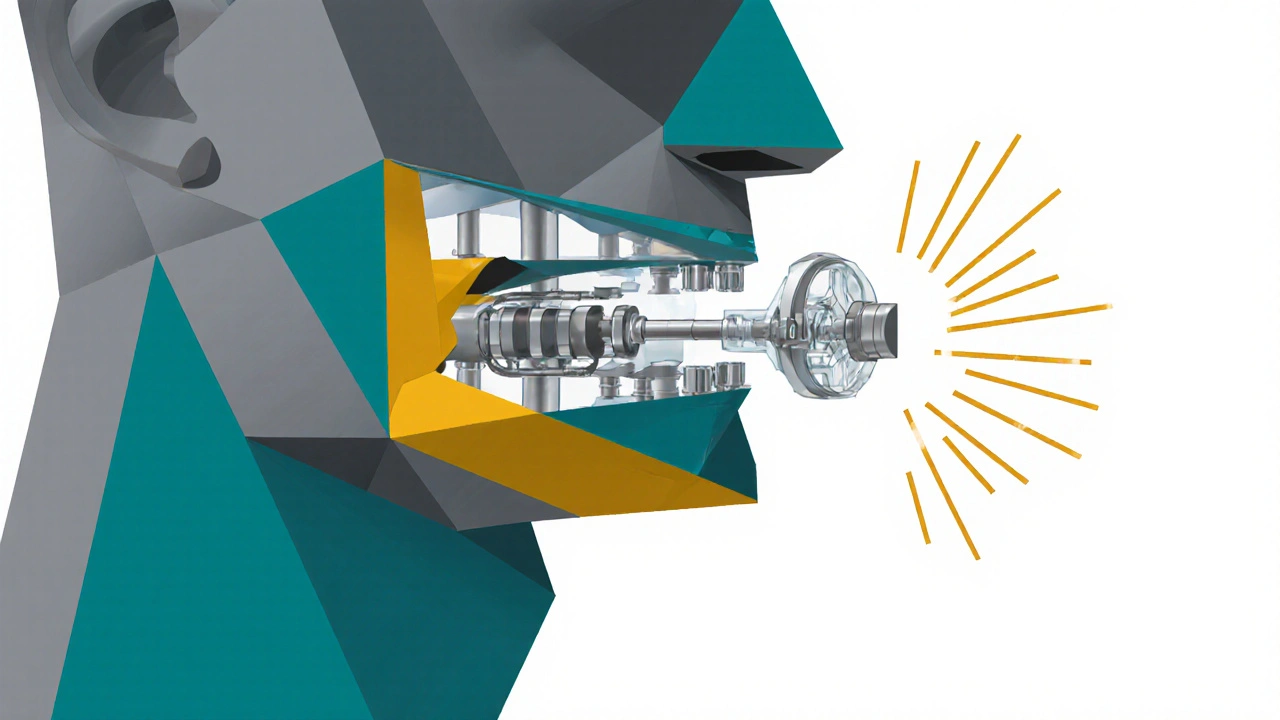
When you sleep, your throat muscles relax. For some people, that causes the tongue and soft tissues to collapse backward, partially blocking the airway. That’s when snoring happens-the vibration of those tissues as air tries to squeeze through. Mandibular advancement devices work by holding your lower jaw in a slightly forward position, which pulls the base of your tongue and surrounding tissues away from the back of your throat. This simple mechanical shift keeps the airway open, reducing or even eliminating snoring.
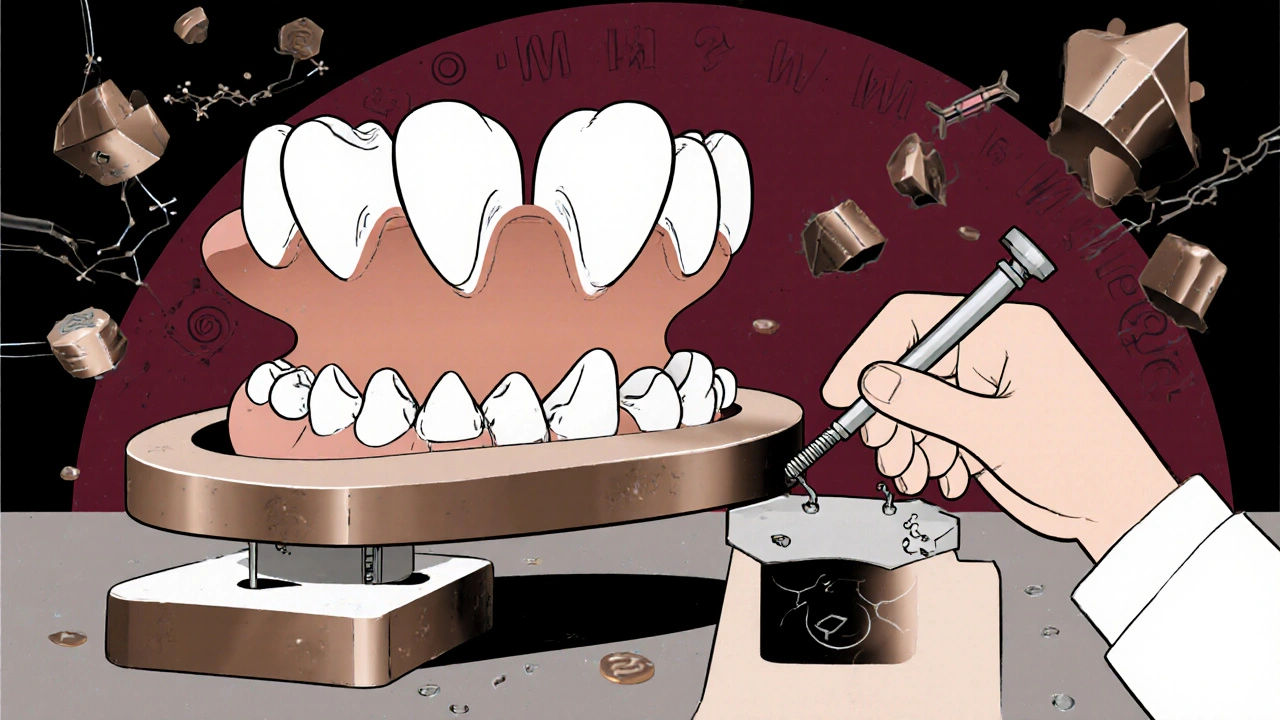
These devices aren’t just guesswork. They’re built on precise science. Studies show that advancing the jaw by 6-10 millimeters from its natural resting position delivers the best results. Too little, and it won’t help. Too much, and you risk jaw pain or damage. That’s why custom-made devices from a dentist are far more effective than over-the-counter boil-and-bite versions. Prescription MADs use semi-rigid acrylic with titanium connectors and allow fine-tuning in 0.5mm increments. You don’t just buy one and hope it works-you adjust it slowly over weeks until snoring stops.
Who Benefits Most from This Treatment?
Not everyone who snores is a good candidate. The best candidates are people with primary snoring (no sleep apnea) or mild to moderate obstructive sleep apnea. If your snoring is loud, frequent, and accompanied by gasping or daytime fatigue, you should get a sleep test first. Severe sleep apnea still requires CPAP, but if you can’t tolerate it, MADs are the next best option.
According to the American Academy of Sleep Medicine, MADs are a first-line treatment for these groups. They’re especially helpful for people who:
- Travel often and find CPAP bulky or inconvenient
- Have mild anatomical narrowing but no complete airway collapse
- Prefer a quiet, portable solution over a machine with a hose and mask
- Have tried positional therapy or nasal dilators with little success
But there are red flags. If you have fewer than 6-8 natural teeth per arch, severe gum disease, or active TMJ pain, MADs might not be safe. About 12.7% of snorers are ruled out due to dental issues. Also, if your airway is completely blocked when lying flat (Mallampati class IV), MADs will likely fail. A dentist trained in sleep medicine will check your mouth, jaw movement, and dental health before recommending one.
Custom vs. Over-the-Counter Devices: The Real Difference
You’ll see ads for $99 snoring mouthpieces on Amazon or TV. They look similar to prescription devices-but they’re not the same. Over-the-counter (OTC) MADs like Zyppah or Good Morning Snore Solution are made from thermoplastic that you soften in hot water and bite into. They’re one-size-fits-most, with fixed advancement of only 3-5mm. That’s not enough for most people.
A 2015 meta-analysis found that custom, titratable MADs reduced snoring by 72.3% on average. OTC devices? Only 48.6%. Why? Because they can’t be adjusted. You can’t fine-tune how far your jaw moves. You can’t increase the advancement if it’s not working. And they often don’t fit well, causing saliva buildup, soreness, or falling out during sleep.
Prescription devices like the SomnoDent MAS or TAP 3 are made from dental impressions taken in-office. They’re designed for your unique bite and jaw shape. Most come with a screw mechanism that lets your dentist slowly increase the jaw position over weeks. That’s the key to long-term success. You don’t just wear it-you optimize it.

What to Expect During Treatment
Getting started isn’t instant. The process usually takes 4-8 weeks:
- You get a sleep test (home or lab) to confirm snoring or mild/moderate sleep apnea.
- You visit a dental sleep specialist for an exam and dental impressions.
- Your custom device is made-this takes 2-3 weeks.
- You start wearing it nightly, adjusting it by 0.5-1mm every few days as directed.
- You return for follow-ups at 2, 4, and 8 weeks to check fit, comfort, and snoring reduction.
Most people notice improvement within the first week. But the first two weeks are often the hardest. You might drool more than usual. Your jaw might feel sore in the morning. Your teeth might feel tender. That’s normal. Dentists recommend wearing the device for an hour or two during the day to get used to it before sleeping. Warm water soaks can help soften the material if adjustments feel stiff.
By day 30, 76% of users are wearing it every night. That’s the magic number-adherence. If you stop using it, snoring comes back within 48 hours. It’s not a cure. It’s a nightly tool.
Side Effects and Long-Term Risks
Yes, there are downsides. About 68% of users report jaw pain or discomfort during the first few weeks. Around 43% experience increased saliva production. A smaller group-about 29%-have ongoing tooth sensitivity or bite changes.
The biggest concern is long-term dental effects. A 2023 study from SUNY found that 25% of long-term users develop irreversible changes in their bite. Some need orthodontic work after 5+ years of use. That’s why regular dental check-ups every 6 months are non-negotiable. Your dentist needs to monitor your teeth, gums, and jaw joints.
Still, for most people, the trade-off is worth it. The alternative-loud snoring that keeps your partner awake, or untreated sleep apnea that raises your risk of high blood pressure, heart attack, and stroke-is far more dangerous. The American Academy of Sleep Medicine says the benefits outweigh the risks for properly selected patients.
Cost, Insurance, and Value
Custom MADs cost between $1,800 and $2,500. That’s steep. But think about it: CPAP machines cost $500-$3,000 too, and you still need to buy masks, tubing, and filters every few months. And CPAP has a 55% dropout rate within a year. MADs? About 76% of users stick with them long-term.
Insurance coverage is spotty. Only 38% of U.S. commercial plans cover MADs as of 2023. Some require proof of failed CPAP therapy. Others only cover them if you have diagnosed sleep apnea-not just snoring. Medicare doesn’t cover them for primary snoring. That means many people pay out of pocket.
But if your snoring is ruining your relationship, your sleep, or your energy, it’s often worth it. One Reddit user shared that his wife measured his snoring dropping from 65 decibels (like a vacuum cleaner) to 38 (like normal conversation). That’s not just comfort-that’s quality of life.
The Future of Snoring Treatment
The field is evolving fast. In 2023, the FDA cleared the SomnoDent EVO 3, the first MAD with built-in sensors that connect to a smartphone app. It tracks how often you wear it and how much you advance your jaw. In 2024, a new device from Sleep Solutions Inc. will use AI to recommend the best jaw position based on your sleep patterns.
Researchers are even exploring genetic markers to predict who will respond best to MADs. The goal isn’t just to stop snoring-it’s to personalize treatment so you get the right device, the right adjustment, and the right outcome the first time.
Is It Right for You?
If you snore loudly and regularly, and you’re tired of living with it-or making your partner miserable-oral appliance therapy is worth exploring. It’s not perfect. It’s not cheap. It requires commitment. But for millions of people, it’s the only thing that finally worked.
Start with a sleep test. Talk to a dentist who specializes in sleep medicine. Don’t settle for a $99 gadget from the internet. If you’re a good candidate, a custom MAD could give you back nights of quiet sleep-and maybe even save your health.
Can oral appliances cure snoring permanently?
No, oral appliances don’t cure snoring permanently. They work only while you wear them. If you stop using the device, snoring typically returns within 48 hours. They manage the condition by keeping your airway open during sleep, not by fixing the underlying anatomy.
Do I need a sleep study before getting a mandibular advancement device?
Yes. A sleep study-either at home or in a lab-is required to rule out moderate or severe obstructive sleep apnea. If you have severe OSA, a CPAP machine is usually the better choice. Even if you think you only snore, a sleep test confirms whether there’s an underlying breathing disorder that needs different treatment.
Are over-the-counter snoring devices effective?
Most over-the-counter devices offer limited help. They’re not custom-fit and can’t be adjusted precisely. Studies show they reduce snoring by only about 48% on average, compared to 72% for custom, titratable devices. They’re better than nothing, but if you’re serious about stopping snoring, a dentist-made appliance is far more reliable.
How long does it take to get used to wearing a mandibular advancement device?
Most people adapt within 10-14 days. Initial side effects like jaw soreness, excess saliva, or tooth pressure are common but usually fade. Dentists often recommend wearing the device for short periods during the day to help your jaw adjust before sleeping with it full-time. By 30 days, most users are wearing it every night without issue.
Can a mandibular advancement device damage my teeth?
Yes, long-term use can cause dental changes. About 25% of users develop bite shifts, tooth movement, or jaw joint discomfort over several years. That’s why regular dental check-ups every 6 months are essential. A dentist trained in sleep medicine can monitor your teeth and make adjustments before permanent damage occurs.
Will my insurance cover a mandibular advancement device?
It depends. Only about 38% of U.S. commercial insurance plans cover these devices, and many require a diagnosis of obstructive sleep apnea-not just snoring. Medicare doesn’t cover them for primary snoring. Always check with your provider before proceeding. Some plans require a trial of CPAP first.



So I tried one of those $99 Amazon gadgets after reading this post-turned out it felt like a mouthful of wet plastic and made me drool like a puppy. Then I went to a sleep dentist, got a custom MAD, and now my wife actually kisses me goodnight instead of throwing pillows. Worth every penny. Also, she’s started sleeping through the night… and so am I. 🙌
November 23Justin Daniel