Polycystic Ovary Syndrome, or PCOS, isn’t just about irregular periods or acne. For many women, it’s a hidden hormonal storm that quietly disrupts fertility, metabolism, and mental health. About 1 in 10 women of childbearing age have it - and half of them don’t even know it. If you’ve been trying to get pregnant for months or years without success, or if your periods have been unpredictable since your teens, PCOS might be the missing piece. The problem isn’t just ovaries covered in cysts - it’s a cascade of hormonal errors that throw off ovulation, insulin balance, and even your body’s stress response.
What’s Really Going On Inside Your Body?
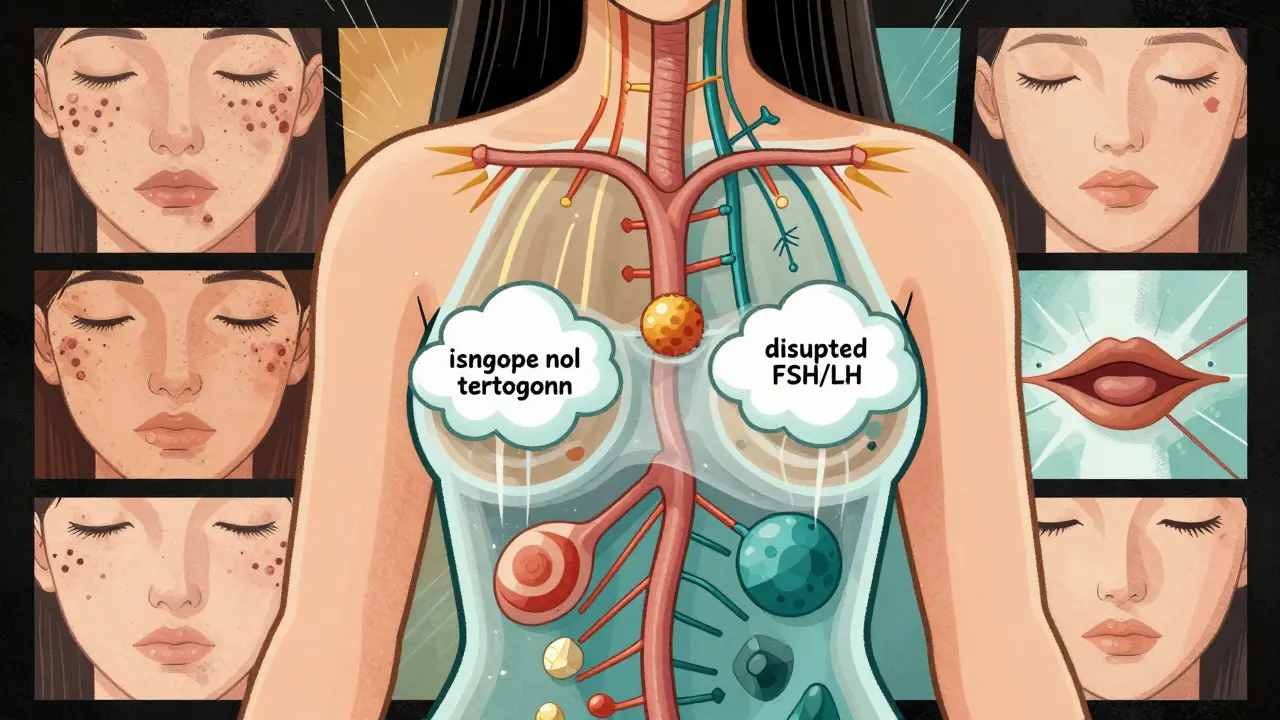
PCOS isn’t one single issue. It’s a mix of three key problems: too many male hormones (androgens), irregular or absent ovulation, and ovaries that look like they’re packed with tiny fluid-filled sacs on an ultrasound. But here’s what most people miss: those cysts aren’t the cause. They’re a side effect. The real trouble starts with insulin resistance.
Up to 70% of women with PCOS have insulin resistance, even if they’re not overweight. That means your body can’t use insulin properly, so it pumps out more to compensate. High insulin levels tell your ovaries to make more testosterone. More testosterone means fewer eggs mature and release each month. It also causes unwanted hair growth, stubborn acne, and thinning hair on the scalp. At the same time, your liver makes less of the protein that binds testosterone, so even more of it floats around freely - making symptoms worse.
Then there’s your brain. The pituitary gland, which controls ovulation, gets confused. It often releases too much luteinizing hormone (LH) and not enough follicle-stimulating hormone (FSH). That imbalance stops follicles from developing properly. No follicle development means no ovulation. And without ovulation, your body doesn’t make enough progesterone. That’s why your periods are erratic or gone - your uterus doesn’t get the signal to shed its lining regularly. Over time, that unopposed estrogen increases your risk of endometrial cancer, which is why untreated PCOS can’t be ignored.
Why Diagnosis Takes So Long - And Why It Matters
On average, women wait over two years to get a proper PCOS diagnosis. Why? Because symptoms are dismissed. Heavy periods? Just stress. Acne? Teenage phase. Weight gain? Just eat less. But PCOS doesn’t care about your willpower. It’s a biological glitch, not a lifestyle failure.
Doctors use the Rotterdam criteria: you need at least two of these three things - irregular periods, signs of high androgens (like facial hair or blood tests showing elevated testosterone), and polycystic ovaries on ultrasound. But here’s the catch: you don’t need all three cysts to have PCOS. And in teens, ultrasounds can be misleading - their ovaries naturally have more follicles. That’s why experts now say not to rely on scans for diagnosis under 18.
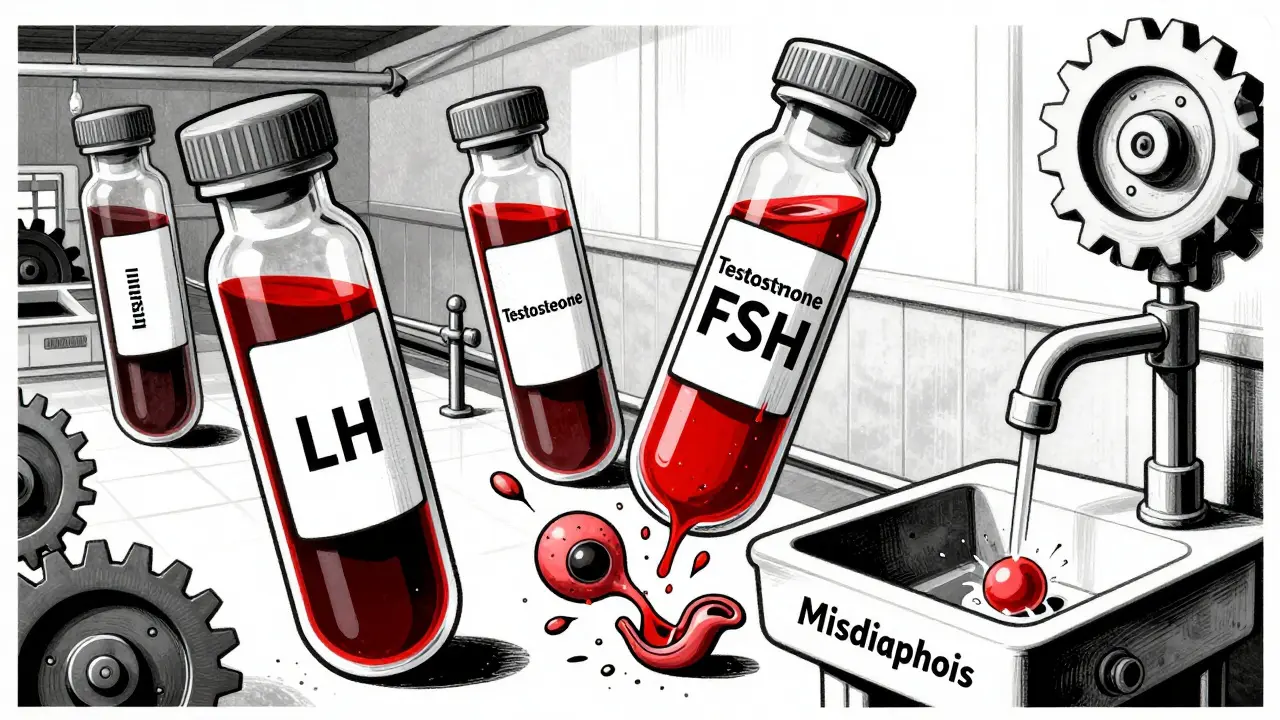
Before calling it PCOS, your doctor should rule out other conditions. Thyroid problems affect up to 20% of women with PCOS-like symptoms. Congenital adrenal hyperplasia, a rare genetic disorder, can mimic PCOS too. Blood tests for TSH, prolactin, and 17-OHP are essential. Skipping these leads to misdiagnosis - and wrong treatment.
Fertility Treatment: What Actually Works
If you’re trying to get pregnant, the goal is simple: get your body to release an egg. And there are proven steps to make that happen.
Step 1: Lifestyle changes - even if you’re not overweight. Losing 5-10% of your body weight can restore ovulation in up to half of women with PCOS. But you don’t need to starve yourself. Focus on low-glycemic foods - beans, oats, berries, leafy greens - that don’t spike insulin. The DASH diet (designed for high blood pressure) has been shown to improve menstrual regularity by 35% in 12 weeks. Add 150 minutes of walking or cycling a week. You don’t need to run marathons. Just move consistently.
Step 2: Clomiphene citrate (Clomid). This is the most common first drug. It tricks your brain into making more FSH, which wakes up the follicles. About 7 out of 10 women ovulate on Clomid. About 3 in 10 get pregnant within six cycles. But it doesn’t work for everyone - about 1 in 4 women don’t respond.
Step 3: Letrozole (Femara). Originally a breast cancer drug, letrozole is now the top choice for PCOS fertility. In a major 2014 trial, women on letrozole had higher ovulation rates (88% vs. 70%) and more live births (27.5% vs. 19.1%) than those on Clomid. It’s now recommended as first-line by major guidelines. It’s cheaper, safer, and more effective. If your doctor pushes Clomid first without mentioning letrozole, ask why.
Step 4: Metformin. This diabetes drug helps with insulin resistance. Alone, it’s not great for getting pregnant - only 15-40% of women ovulate on it. But when paired with Clomid or letrozole, it boosts pregnancy rates by 30-50%, especially if your BMI is over 35. Side effects? Nausea and diarrhea. Start low (500 mg/day), increase slowly, and take it with food. Most people adjust within a few weeks.
Step 5: Gonadotropins and IVF. If oral meds fail, injections of FSH and LH (gonadotropins) can force ovulation. Success rates are 15-20% per cycle, but the risk of twins or triplets jumps to 20-30%. Ovarian hyperstimulation syndrome (OHSS) happens in 5-10% of cases - a dangerous swelling of the ovaries. IVF is usually saved for when there are other infertility issues, like blocked tubes or male factor. But PCOS patients need lower doses of meds during IVF to avoid OHSS. Still, your risk is double that of non-PCOS patients.
What Doesn’t Work - And Why
There’s a lot of noise out there. You’ll hear about cinnamon, spearmint tea, or acupuncture curing PCOS. Some of these might help a little with symptoms, but none restart ovulation reliably. Don’t waste money on unproven supplements. Stick to what’s backed by large, peer-reviewed studies.
Also, don’t assume weight loss is the only answer. Thin women get PCOS too. Insulin resistance isn’t tied to body size. A woman with a BMI of 21 can have the same hormonal chaos as someone with a BMI of 35. Treatment should focus on your hormones and insulin, not just the scale.
The Bigger Picture: PCOS Is Lifelong
Getting pregnant isn’t the end of the story. Women with PCOS are two to four times more likely to develop type 2 diabetes by age 40. Heart disease risk is doubled. High blood pressure and cholesterol are common. That’s why annual blood tests for glucose, HbA1c, and lipids aren’t optional - they’re life-saving.
And mental health? Depression and anxiety affect up to half of women with PCOS. The constant cycle of failed cycles, body image struggles, and being told it’s "all in your head" takes a toll. Therapy, support groups, and even apps like Femaloop (FDA-approved for PCOS) can help manage stress - which itself worsens hormonal imbalance.
There’s new hope on the horizon. Trials are underway for drugs like relugolix, which can normalize cycles without suppressing fertility. AI tools are being trained to predict PCOS from hormone levels and ultrasound images with over 90% accuracy. But the most powerful tool remains: early diagnosis and consistent, coordinated care.
What To Do Next
If you suspect PCOS, start with these three steps:
- Get blood work: Test testosterone, LH, FSH, insulin, fasting glucose, HbA1c, TSH, and prolactin.
- Track your cycles: Use an app or calendar. Note when you bleed, if you have ovulation pain, or if you notice cervical mucus changes.
- See a specialist: Not all OB-GYNs are trained in PCOS. Look for a reproductive endocrinologist or an endocrinologist with PCOS experience.
Don’t wait for a crisis. If you’re not getting your period for three months or more, or if you’ve been trying to conceive for over a year (or six months if you’re over 35), get checked. PCOS is manageable. It’s not curable, but with the right approach, you can ovulate, get pregnant, and protect your long-term health.
Can you get pregnant with PCOS without treatment?
Yes, but it’s less likely. About 30% of women with PCOS conceive naturally within a year without intervention. But if you’re not ovulating regularly, your chances drop significantly. Treatment improves ovulation rates from under 20% to 60-88%, making pregnancy far more predictable.
Does metformin help with weight loss in PCOS?
Metformin can help some women lose 2-5% of body weight over six months, mainly by reducing insulin spikes and appetite. But it’s not a weight-loss drug. Its main benefit is improving insulin sensitivity, which helps ovulation and lowers diabetes risk. Weight loss still requires diet and movement.
Is letrozole safer than Clomid for PCOS?
Yes. Letrozole has fewer side effects like mood swings and thinning uterine lining, which can lower pregnancy chances with Clomid. It’s also more effective at triggering ovulation and leading to live births. Major guidelines now recommend letrozole as the first drug for PCOS infertility, not Clomid.
Can PCOS be cured?
No, PCOS can’t be cured - but it can be managed. With lifestyle changes, medication, and regular monitoring, symptoms can be controlled, fertility restored, and long-term risks like diabetes and heart disease reduced. Many women live symptom-free for years once they find the right combination of treatments.
Why do some women with PCOS have regular periods?
Not all PCOS looks the same. Some women have milder hormonal imbalances and still ovulate occasionally. Others have normal periods but still have high androgens and insulin resistance. These are called "non-ovulatory PCOS" or "phenotype C" under the Rotterdam criteria. You don’t need irregular periods to have PCOS - you just need two of the three features.
PCOS doesn’t define you. But ignoring it does. The right care - grounded in science, not myths - gives you back control. Start with your doctor. Ask the right questions. And don’t stop until you get answers that make sense.





i had no idea insulin resistance was the real culprit behind my acne and hair growth. i thought it was just bad skincare and stress. got tested last year and yep-high insulin, normal weight. this post literally changed my life. started eating oats and berries and my periods are actually regular now. no meds, just food. weird, right?
January 7Patty Walters