Prior Authorization: What It Is, Why It Matters, and How to Navigate It
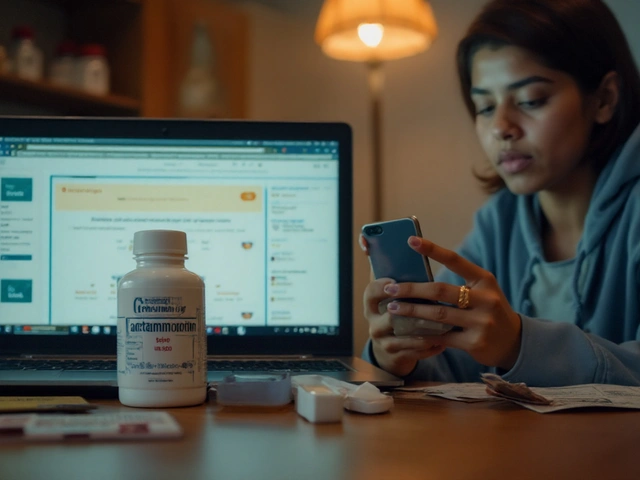
When your doctor prescribes a medication, but your insurance says prior authorization, a process where insurers require approval before covering certain drugs. Also known as pre-authorization, it's not a medical decision—it's a financial gatekeeping step built into most health plans. You’re not alone if you’ve waited days or weeks for a simple prescription to be approved. This isn’t about safety—it’s about cost control. Insurers use prior authorization to push you toward cheaper alternatives, even if your doctor knows the prescribed drug works best for you.
Prior authorization isn’t random. It targets high-cost drugs like specialty cancer treatments, biologics for autoimmune diseases, or even common meds like certain diabetes or migraine pills. It also applies to things like durable medical equipment, physical therapy, or lab tests. The system was designed to stop overuse, but in practice, it often delays care. A 2023 study by the American Medical Association found that 93% of physicians reported prior authorization caused treatment delays, and 78% said it led to patients abandoning needed meds altogether. You might think your pharmacy handles it, but more often, your doctor’s office is stuck filling out forms, calling insurers, and waiting for responses that come back days later—sometimes after your prescription has expired.
Some drugs are on a blacklist—meaning they require prior authorization every single time, even if you’ve taken them for years. Others are only approved if you’ve tried and failed cheaper versions first, a process called step therapy. This is where things get messy. What if the cheaper drug gave you nausea, or made your condition worse? Insurers don’t always listen. You might need a letter of medical necessity, lab results, or even a second opinion to get approval. And if you’re on Medicare Advantage or a private plan, the rules change by state, by insurer, even by pharmacy network.
That’s why the posts below matter. You’ll find real stories and practical guides on how to fight back: how to spot when prior authorization is being misused, how to write a letter that actually gets approved, what to do when your drug gets denied, and how to avoid getting caught in the loop when switching plans. You’ll also learn how certain meds—like those used for osteonecrosis of the jaw, COPD, or HIV—are especially likely to trigger these delays. And if you’re managing chronic conditions, you’ll see how prior authorization affects everything from your sleep (melatonin), your heart (Hepatitis C-related risks), to your daily routine (metformin, tiotropium, or even ginseng supplements). This isn’t just paperwork. It’s about getting the right treatment at the right time.