Cognitive Decline in Elderly: Signs, Risks, and Medication Risks to Watch For
When we talk about cognitive decline in elderly, a gradual loss of thinking skills like memory, focus, and decision-making that affects daily life. Also known as mild cognitive impairment, it’s not a normal part of aging—it’s a warning sign that something else is going on. Many people assume forgetfulness is just getting older, but when it starts interfering with paying bills, taking meds, or remembering appointments, it’s time to look deeper.
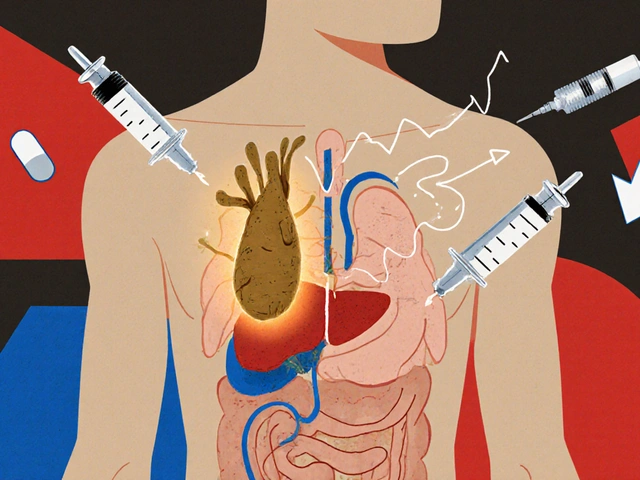
One of the biggest hidden drivers of cognitive decline in seniors is medication interactions, when multiple drugs clash in the body and disrupt brain function. Think about an older adult taking blood pressure pills, painkillers, sleep aids, and cholesterol meds—all processed by the same liver enzymes. That’s where CYP450 inhibition, a process where certain substances block how the body breaks down drugs comes in. CBD oil, grapefruit juice, even some antibiotics can slow down drug metabolism, causing sedation, confusion, or even overdose. A 78-year-old on statins and a sleep med might start zoning out not because of aging, but because their liver can’t keep up.
It’s not just about what you take—it’s about what you don’t stop taking. polypharmacy, the use of five or more medications at once is common in seniors, and it’s a major risk factor for brain fog. Studies show that up to 40% of older adults on multiple prescriptions show signs of cognitive slowdown linked directly to drug burden. Some meds—like anticholinergics used for allergies, overactive bladder, or depression—directly block acetylcholine, a key brain chemical for memory. These drugs are often prescribed for years without review, even though they’re on lists of medications to avoid in seniors.
And then there’s the silent link between chronic inflammation and brain health. Conditions like rheumatoid arthritis, which require long-term use of immunosuppressants, drugs that dampen the immune system to control autoimmune damage, can increase systemic inflammation. That inflammation doesn’t just attack joints—it can cross into the brain and speed up neurodegeneration. It’s not just about treating the disease; it’s about asking if the treatment is helping or hurting the mind.
What’s surprising is how often simple fixes make a difference. Bringing actual pill bottles to doctor visits cuts medication errors by 67%. Asking your pharmacist to review your list isn’t a nuisance—it’s a brain-saving habit. Skipping grapefruit juice, avoiding unnecessary sleep aids, and checking if a drug is on the Beers List of potentially inappropriate meds for seniors can do more than any supplement ever could.
You won’t find a magic pill to reverse cognitive decline, but you can stop the things that make it worse. The posts below dive into the real connections between everyday medications and brain health—what to watch for, what to question, and what to ask your doctor before the next prescription hits the bottle.