Pharmaceutical Patents: What They Are, Why They Matter, and How They Shape Your Medications
When you pick up a prescription, what you’re holding might be protected by a pharmaceutical patent, a legal monopoly granted to drug companies to exclusively make and sell a new medication for a set period. Also known as drug exclusivity, it’s the reason brand-name drugs cost so much—and why, eventually, cheaper versions show up on pharmacy shelves. This isn’t just a legal detail. It’s the engine behind how new medicines get made, how long you pay high prices, and when your doctor can switch you to a generic.
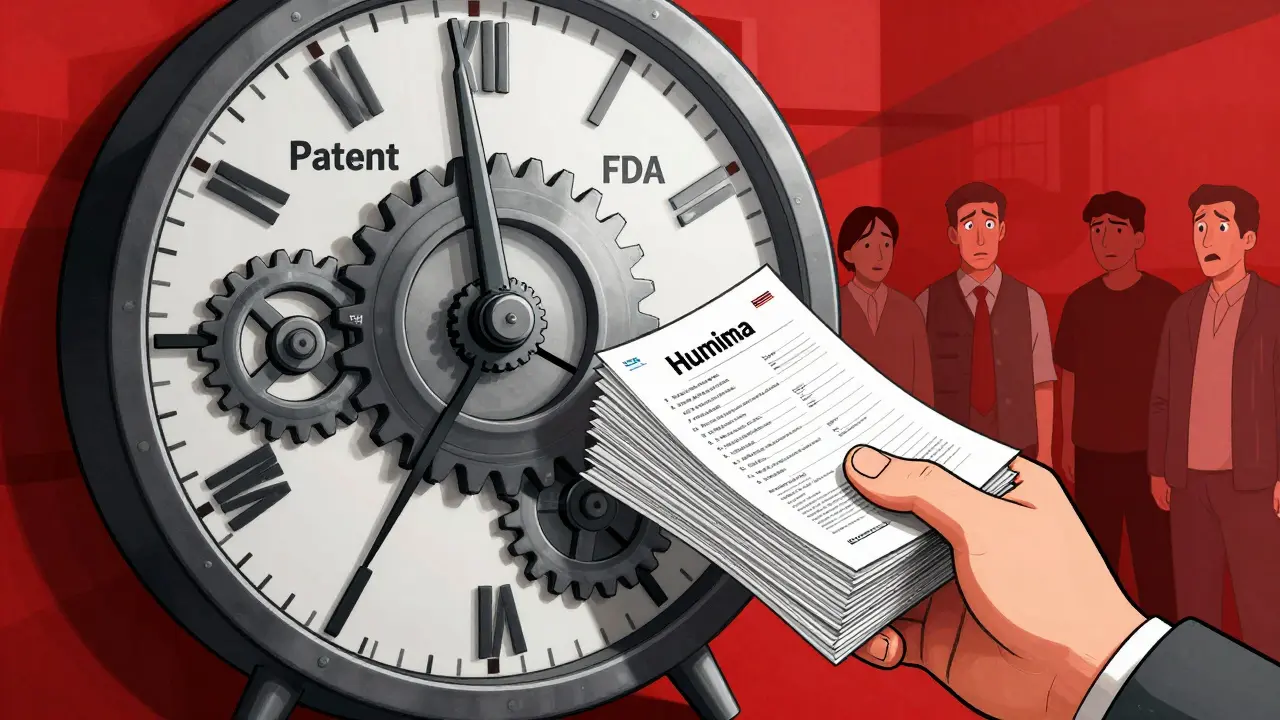
Pharmaceutical patents are tied directly to FDA approval, the official process that confirms a drug is safe and effective for public use. A company can’t even apply for a patent until they’ve proven their drug works. Once approved, they get up to 20 years of patent protection, but that clock often starts ticking before clinical trials even begin. By the time the drug hits shelves, only 7–12 years of exclusivity may remain. That’s why companies file multiple patents—on formulations, dosages, delivery methods, even packaging—to stretch their market control. This is why some drugs stay expensive for years, even after the original patent expires.
When that exclusivity ends, generic drugs, medications that contain the same active ingredient as the brand-name version at a fraction of the cost flood the market. But it’s not automatic. Generic makers must prove their version is bioequivalent—meaning your body absorbs it the same way. That’s why some people notice differences in how a generic works, even if the label says it’s identical. The gap between patent expiration and generic availability can mean big savings—or big headaches—if delays happen due to legal battles or manufacturing issues.
That’s where things get messy. Some drugmakers use tactics like "patent thickets"—filing dozens of minor patents—to block generics. Others delay approvals by suing generic companies, a practice called "pay-for-delay," where the brand pays the generic maker to stay off the market. These aren’t just corporate tricks. They affect your wallet, your access to treatment, and even whether you stick with your meds because you can’t afford them.
What you’ll find in this collection are real-world stories about how patents shape your health. You’ll read about how patent rules impact the price of your insulin, why some drugs never go generic, how pharmacists spot counterfeit pills tied to expired patents, and why your doctor might switch you to a different drug just before a patent expires. You’ll also see how patient registries and drug safety programs track outcomes once generics arrive, and how traveling with refrigerated meds can get complicated when patent protections limit which versions are available abroad.
Pharmaceutical patents aren’t abstract legal terms. They’re the invisible hand behind every pill you take. Whether you’re managing arthritis with biologics, taking a blood thinner like enoxaparin, or using CBD oil that interacts with your prescriptions, the patent status of your meds affects what’s available, how much you pay, and how safe your treatment is. Below, you’ll find practical guides that cut through the noise and show you exactly how this system impacts your daily life—and what you can do about it.