Medication Safety in 2025: FDA Recalls, Drug Interactions, and Safe Use Guide
When it comes to your health, medication safety, the practice of using drugs correctly to avoid harm, injury, or death. Also known as drug safety, it’s not just about taking pills as directed—it’s about understanding what’s in them, how they react with other substances, and what to do when something goes wrong. In 2025, this isn’t theoretical. It’s daily reality for millions. The FDA recall process, the system the U.S. Food and Drug Administration uses to remove unsafe drugs from shelves. Also known as drug recall authority, it doesn’t force companies to pull products—it asks them. And when they don’t act fast enough, patients pay the price. That’s why knowing how recalls work, who’s responsible, and what to do if your medicine is pulled isn’t just helpful—it’s life-saving.
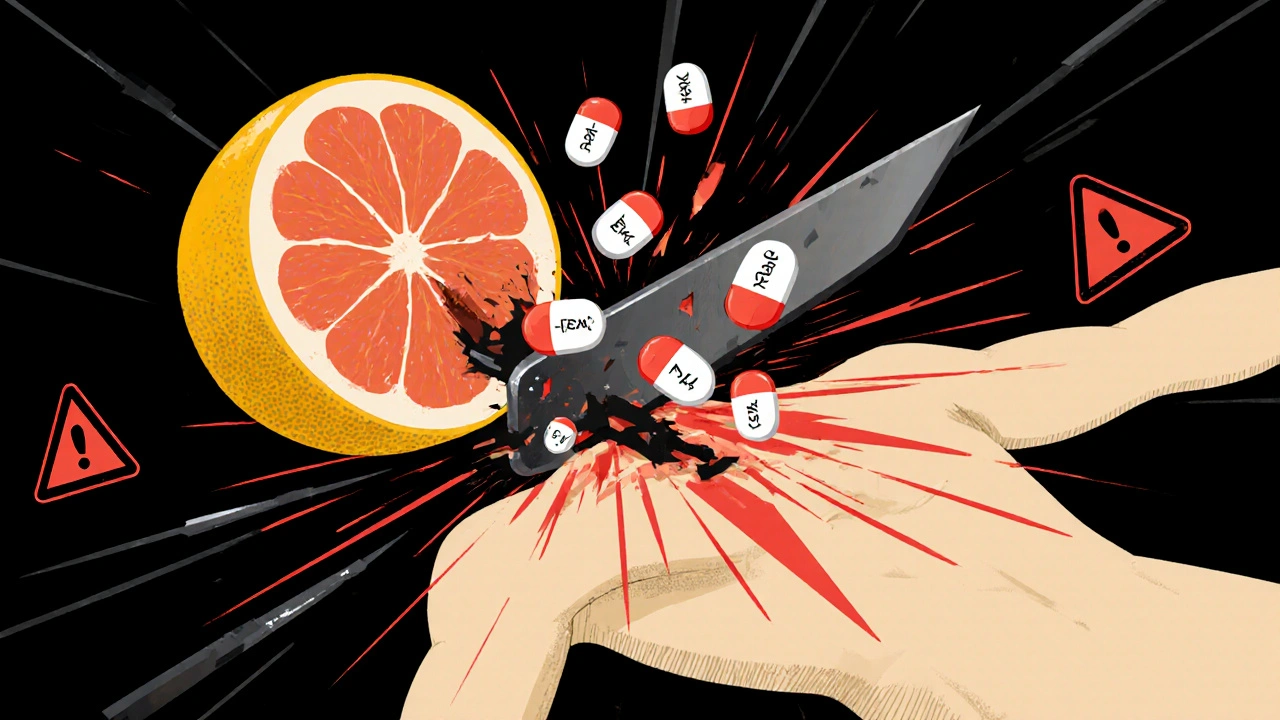
Drug interactions, harmful reactions between medications, food, or supplements. Also known as medication interactions, they’re one of the top causes of hospital visits. Grapefruit juice isn’t just a breakfast staple—it can spike your blood pressure meds or statins to dangerous levels. Ginseng might seem natural and safe, but it can crash your blood sugar if you’re on insulin. Even something as simple as splitting a pill can lead to contamination or wrong doses if you don’t know how. And let’s not forget pets—human medications are the #1 cause of pet poisonings. A single Tylenol tablet can kill a cat. A few antidepressant pills can send a dog to the ER.
That’s why patient registries, voluntary programs that track how drugs affect real people over time. Also known as medication monitoring, they’re quietly saving lives. These aren’t just government databases—they’re tools you can join to help researchers spot dangers before they spread. If you’re on a drug linked to rare side effects like jaw bone death or liver damage, your enrollment helps update guidelines and warn others.
And then there’s the opioid crisis. In 2025, doctors are told to avoid prescribing them unless absolutely necessary. New rules require risk checks before every script. But pain doesn’t disappear just because the pills do. That’s why opioid safety, strategies to prevent addiction, overdose, and misuse. Also known as pain management, it’s now about combining nerve blocks, physical therapy, and non-addictive meds. It’s not about going cold turkey—it’s about smarter, safer ways to feel better.
What you’ll find here isn’t theory. It’s real advice from real cases. How to keep insulin cold on a road trip. Why bringing your pill bottles to appointments cuts errors by two-thirds. How to spot the warning signs of pancreatitis hiding as heartburn. What to do if your glaucoma meds need to be stopped. And how melatonin isn’t a sleeping pill—it’s a signal. Each article answers a question someone actually asked, in a way they can use tomorrow.